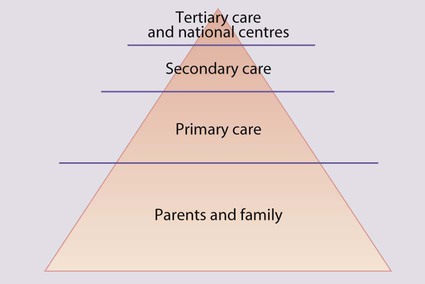
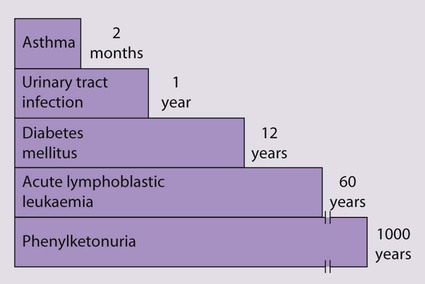
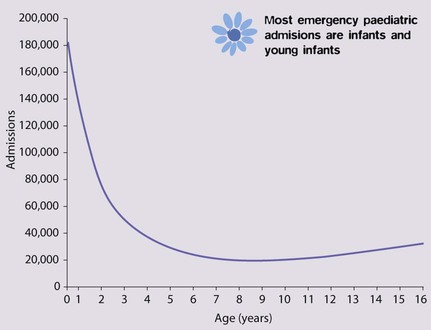
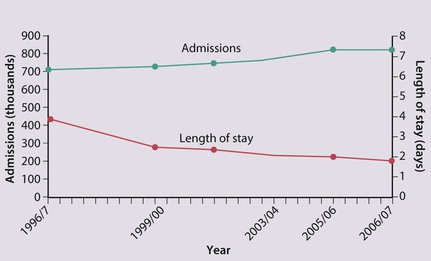
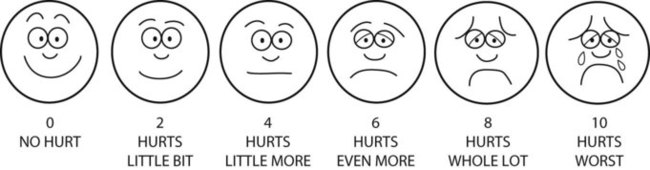
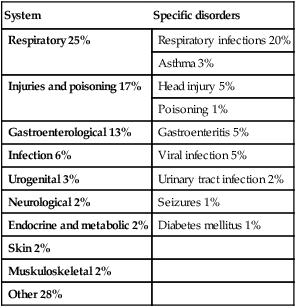
Most sick children are cared for by their parents at home. Medical management is initially given by general practitioners or, in some countries, primary care paediatricians. Most hospital admissions are at secondary care level. A smaller number of children will require tertiary care in a specialist centre, e.g. paediatric intensive care unit, cardiac or oncology unit. Most specialist centres now share care within clinical networks, with the centre linked to a number of surrounding hospitals. For very rare and complex treatments, e.g. organ transplantation and craniofacial surgery, there are a few national centres (Fig. 5.1). The majority of acute illness in children is mild and transient (e.g. upper respiratory tract infection, gastroenteritis) or readily treatable (e.g. urinary tract infection). Although serious conditions are uncommon (Fig. 5.2), they must be identified promptly. The condition of sick children, especially infants, may deteriorate rapidly, and parents require rapid access to a general practitioner or other healthcare professionals working in primary care, who in turn require ready access to secondary care. Advice may also be obtained from a health professional by telephone, e.g. via NHS Direct, via the internet with NHS Direct Online or by NHS Direct cable TV services. Although an individual general practitioner will care for relatively few children with serious chronic illnesses (e.g. cystic fibrosis, diabetes mellitus) or disability (e.g. cerebral palsy), each affected child and family are likely to require considerable input from the whole of the primary care team. Approximately 3 million children (1 in 4) attend an Accident and Emergency (A&E) department each year in England and Wales. The services which should be provided for children are shown in Box 5.1. The number of departments able to meet these expectations is increasing, often by creating a dedicated children’s A&E department. In England and Wales, 1.9 million, i.e. 1 in 6 children is admitted to hospital each year, representing 16% of all hospital admissions. About 60% of acute admissions are under the care of paediatricians, and the remainder are surgical patients (although a paediatrician is also involved in their care while they are in hospital, to oversee any medical requirements) (Fig. 5.3). Most paediatric admissions are of infants and young children under 5 years of age and are emergencies, whereas surgical admissions peak at 5 years of age, one-third of which are elective. The reasons for medical admission are shown in Table 5.1. Table 5.1 Reason for emergency admission of children <15 years old to hospital Data based on 58 061 admissions, 2009–2010. ISD, Scotland. Although primary and community health services for children have improved markedly over the last decade, the hospital admission rate has continued to rise, although it may now be plateauing (Fig. 5.4). The reasons for this are unclear, but probably include: • Lower threshold for admission: there appears to be an increased expectation of hospital admission by parents and medical staff worried that the child’s clinical condition may deteriorate • Repeated hospital admission of children with complex conditions who would have died in the past but are now surviving, e.g. very low birthweight infants from neonatal intensive care units, children with cancer or organ failure. Strenuous efforts are made to reduce the rate and length of hospitalisation (Fig. 5.4): • Speciality of ambulatory paediatrics has been developed; it encompasses specialist paediatricians providing hospital care for immediate medical problems outside inpatient paediatric wards • Dedicated children’s short stay beds within or alongside the A&E department are increasingly available to allow children to be treated or observed for a number of hours and discharged home directly, avoiding the need for admission to the ward • Day-case surgery has been instituted for many operations which used to require overnight stay. • Day units are used for complex investigations and procedures instead of inpatient wards • Shared care may be provided between hospitals and primary care, with paediatricians and other healthcare professionals seeing children at home or in primary care settings • Homecare teams aim to provide care in the child’s home and thereby reduce hospital attendance, admission and length of stay. Most teams comprise community paediatric nurses, but some include doctors, and either cover all aspects of paediatric care within a geographical area or are for a specific condition, e.g. cystic fibrosis or malignancy, usually centred around a tertiary referral centre. The problems managed at home by such teams include: – Changing postoperative wound dressings or managing burns – Day-to-day management and support for the family for chronic illnesses, e.g. diabetes mellitus, asthma and eczema – Specialist care, e.g. home oxygen therapy, intravenous infusions via a central venous catheter (e.g. antibiotics or chemotherapy) or peritoneal dialysis – Symptom and pain control and emotional support of terminally ill children (Fig. 5.5) • Children’s hospices provide respite or terminal care for children with life-threatening conditions, including malignancy disease, neurodegenerative, metabolic and other disorders. • Some teams provide a ‘hospital at home’ service for children who are acutely ill, in order to avoid hospitalisation. Older children can describe the nature and severity of the pain they are experiencing. In younger children, assessing pain is more difficult. Observation and parental impression are commonly used and a number of self-assessment tools have been designed for children over 3 years old (Fig. 5.6). The approaches to pain management are listed in Box 5.2. This should allow pain to be prevented or kept to a minimum. Age-appropriate explanation should be given when possible and the approach be reassuring; however, it is imperative not to lie to children, otherwise they will lose trust in what they are told in the future. Distraction techniques such as blowing bubbles, telling stories, holding family toys or playing computer games, as well as the involvement of trained play specialists, can be highly successful in ameliorating pain in children. Some children develop particular preferences for a particular venepuncture site or distraction technique, and this should be accommodated as far as possible.
Care of the sick child
Primary care
Hospital care
Accident and Emergency
Hospital admission
System
Specific disorders
Respiratory 25%
Respiratory infections 20%
Asthma 3%
Injuries and poisoning 17%
Head injury 5%
Poisoning 1%
Gastroenterological 13%
Gastroenteritis 5%
Infection 6%
Viral infection 5%
Urogenital 3%
Urinary tract infection 2%
Neurological 2%
Seizures 1%
Endocrine and metabolic 2%
Diabetes mellitus 1%
Skin 2%
Muskuloskeletal 2%
Other 28%
Pain
Chronic pain
Management