23
Bones and joints
Chapter map
Concerns about bones and joints are common. This chapter reviews common variations in structure and posture, and the different causes of bone and joint pain or dysfunction (including infection, inflammation, and necrosis).
23.1 Structural variation and congenital abnormalities
23.1.3 Knock knees (genu valgum)
23.1.7 Developmental dysplasia of the hip (DDH)
23.1.8 Osteogenesis imperfecta
23.3.1 Irritable hip (transient synovitis)
23.3.3 Joint hypermobility syndrome
23.3.4 Other collagen diseases
23.3.5 Henoch–Schönlein purpura (anaphylactoid purpura)
23.4 Osteochondritis and epiphysitis
23.4.2 Osgood–Schlatter disease
23.5 Slipped upper femoral epiphysis
23.1 Structural variation and congenital abnormalities
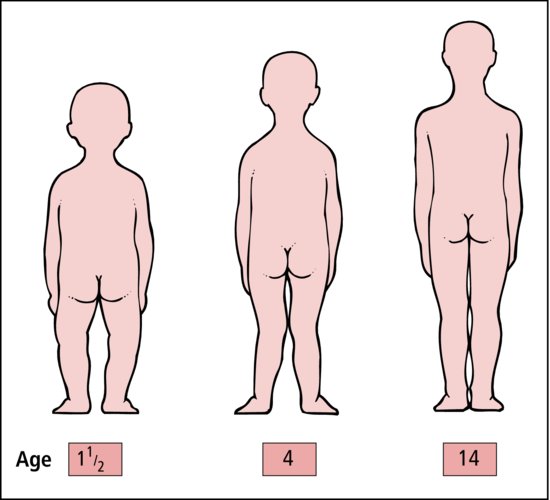
The normal flat-footed baby becomes a bow-legged toddler and then a knock-kneed primary schoolchild before growing into a graceful adolescent. It is important to recognize normal variation and problems requiring investigation and treatment (Figure 23.1).
Examine the child:
- Standing and lying
- Walking and running
- Limb lengths
- Scars
- Muscle wasting
- Uneven wear of shoes.
23.1.1 Flat feet
At birth the feet look flat. A child’s feet continue to look flat as a toddler. By the third year the feet begin to appear to have a normal plantar arch.
23.1.2 Bow legs (genu varum)
Bow legs are most common from 0 to 2 years. The knees may be 5 cm apart when the feet are together: the toes point medially. Marked bowing may mean rickets (Section 12.4.2.4).
23.1.3 Knock knees (genu valgum)
This is most apparent at 3–4 years of age. When the knees are together, the medial tibial malleoli may be up to 5 cm apart. In obese children, the separation may be even greater but, by the age of 12, the legs should be straight. Separation of over 10 cm or unilateral knock knee requires an X-ray and, probably, a specialist opinion.
23.1.4 Intoeing
This is usually a normal variation and resolves by the age of 8 years.
23.1.5 Scoliosis
- Idiopathic (95%)
- Vertebral anomalies, e.g. hemivertebrae
- Muscle weakness, e.g. cerebral palsy.
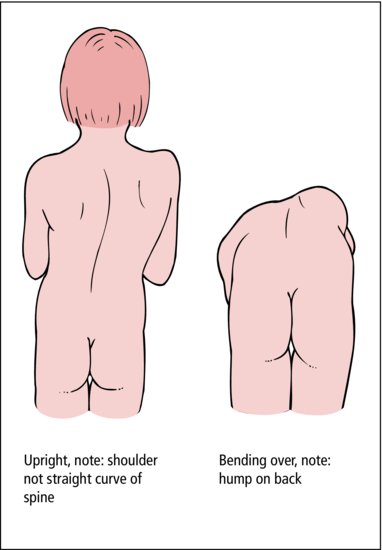
Postural scoliosis is commonly seen in babies: it goes when the baby is suspended and has completely gone by the age of 2 years. Scoliosis is again common at adolescence, especially in girls. If it is postural, it disappears on bending forward. Structural scoliosis produces asymmetry on bending: a hump on flexion (Figure 23.2). Asymmetry of scapulae and shoulders may be more conspicuous than the spinal curve.
 PRACTICE POINT
PRACTICE POINT23.1.6 Talipes (club foot)
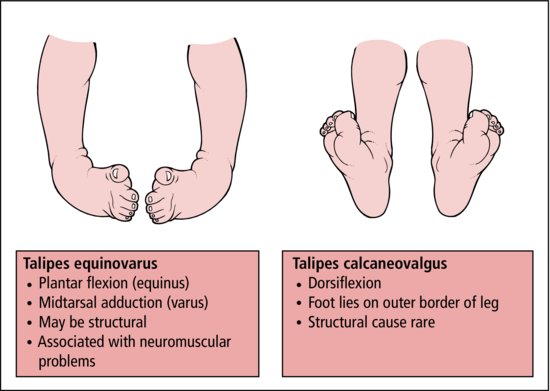
Postural talipes is common at birth, resulting from the fetal foot position in utero. If the foot with talipes equinovarus can be fully dorsiflexed and everted so that the little toe touches the outside of the leg without undue force, it is postural and will get better. Structural talipes cannot be corrected. Early orthopaedic referral is needed for splintage or surgery. The sooner treatment is begun the better the outcome. Talipes calcaneovalgus is usually easily corrected by simple exercises (Figure 23.3).
23.1.7 Developmental dysplasia of the hip (DDH)
DDH is also known as congenital dislocation of the hips. Acetabular dysplasia is important in causation.
- Breech
- Positive family history
- Girls > boys
- Neuromuscular or joint problem (e.g. spina bifida, talipes).
All babies should be examined in the neonatal period for DDH (OCSE station 23.1). Examination is repeated at infant health checks. If there is clinical suspicion or the infant is high risk, hip ultrasound is more reliable than clinical examination. X-ray is unreliable in the first months because of poor ossification.
- 1% of babies have some developmental dysplasia or hip instability
- 1 in 1000 have severe congenital dislocation
- early treatment with splinting in full abduction is successful in most
- late presentation with a limp has a poor prognosis, needing surgery and predisposing to early osteoarthritis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree