CHAPTER 8 acute inflammation of the gallbladder. opening in the duodenum for the entrance of the common bile duct. roundworm that inhibits the intestine. yellow pigment in bile formed by the breakdown of red blood cells. partial or complete absence of the biliary system. an extrahepatic collection of extravasated bile from trauma, surgery, or gallbladder disease. a segmental, saccular, or beaded appearance to the intrahepatic biliary ducts. inflammation of the gallbladder. cystic dilatation of the common bile duct. calculus in the common duct; stones contain bile pigments, bile calcium salts, and cholesterol. type of cholesterolosis associated with a strawberry appearance to the gallbladder. recurrent attacks of acute cholecystitis. term used to include the extrahepatic common hepatic duct and common bile duct. small duct that drains the gallbladder. gas in the gallbladder wall or lumen. small posterior pouch near the gallbladder neck. fold or septation of the gallbladder at the junction of the neck and body. carcinoma located at the junction of the right and left hepatic ducts. fold in the gallbladder fundus. a soft tissue mass protruding from the gallbladder wall. calcification of the gallbladder wall. echogenic bile; viscous bile; contains calcium bilirubinate. mobile, echogenic, nonshadowing mass in the dependent portion of the gallbladder. echogenic bile that does not layer evenly; resembles a polypoid mass. wall-echo-shadow sign; “double arc” sign; seen with a stone-filled gallbladder. • The biliary system originates in the liver as a series of ductules coursing between the liver cells. • Biliary ducts are subdivided into intrahepatic and extrahepatic ducts. • Intrahepatic ducts follow the course of the portal veins and hepatic arterial branches. • The main right and left hepatic ducts lie anterior to the corresponding portal venous trunk. • Extrahepatic ducts include the cystic and common ducts. • Bile flows if intraductal pressure is lower than the hepatic secretory pressure. Pressure differences are affected by the activity of the sphincter of Oddi, filling and resorption of the bile in the gallbladder, and the bile flow from the liver. • Average intraluminal diameter of the CHD is 4 mm and should not exceed 6 mm in adults. • Average intraluminal diameter of the CBD is 6 mm in diameter or less in adults. • Starting at age 60, the CBD may increase in diameter by 1 mm per decade. • Postcholecystectomy patients may demonstrate a slight increase in diameter but should not exceed 10 mm. • Average intraluminal diameter of the CBD is less than 4 mm in children, less than 2 mm in infants up to 1 year, and less than 1 mm in neonates. • The CBD will decrease in size or remain unchanged after a fatty meal. • Anechoic nonvascular tubular structures coursing within the hepatic parenchyma. • Normal intraluminal diameter of the CHD. • The right and left hepatic bile ducts generally lie anterior to the corresponding portal vein. • Intrahepatic bile ducts are not routinely visualized on ultrasound. • The normal fasting adult gallbladder measures approximately 8 to 10 cm in length and 3 to 5 cm in diameter. • The normal fasting pediatric gallbladder measures approximately 1.5 to 3.0 cm in length and 1.2 cm in width in infants less than 1 year of age, and 3 to 7 cm in length and 1 to 3 cm in diameter in children between 2 and 16 years of age. • Nothing by mouth (NPO) 6 to 8 hours before examination for adults, 6 hours for children, and 4 hours for infants. • Appointments are typically made at the beginning of the patient’s day. • Emergency examinations may be performed without preparation. • Use the highest-frequency abdominal transducer possible to obtain optimal resolution for penetration depth. • Place gain settings to display the normal liver parenchyma as a medium shade of gray with adjustments to reduce echoes within the vessels. • Focal zone(s) at or below the place of interest. • Sufficient imaging depth to visualize structures immediately posterior to the region of interest. • Harmonic imaging and decreasing the compression (dynamic range) can be used to reduce artifactual echoes within anechoic structures and improve prominence of posterior acoustic shadowing. • Spatial compounding can be used to improve visualization of structures posterior to a highly attenuating structure. • Begin with the patient in the supine position. • Intrahepatic ducts, extrahepatic ducts, gallbladder, and pancreas should always be evaluated. • After the supine evaluation, the patient is positioned in the oblique, decubitus, or erect views to demonstrate mobility of gallstones or avoid obscuring bowel gas patterns. • Systematic approach to evaluate and document the intra- and extrahepatic ducts, gallbladder, and pancreas in both the longitudinal and transverse planes using specific anatomical landmarks. • Intraluminal measurement and images of the common hepatic and common bile ducts must be documented. (Only the inner diameter is measured.) • In the jaundice patient, careful evaluation of the intrahepatic ducts is warranted. • Color Doppler imaging, using a 60-degree angle or less to distinguish vascular structures from the intrahepatic and extrahepatic biliary tree and to evaluate structures within or around the gallbladder. • Documentation and measurement of any abnormality in two scanning planes should be included.
Biliary system
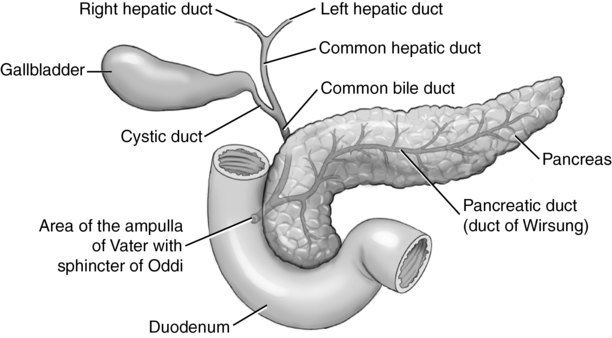
Biliary anatomy (fig. 8-1)
Bile ducts
Size of the normal bile duct
Sonographic appearance
Normal intrahepatic bile ducts
Gallbladder size
Technique
Preparation
Examination technique and image optimization
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree