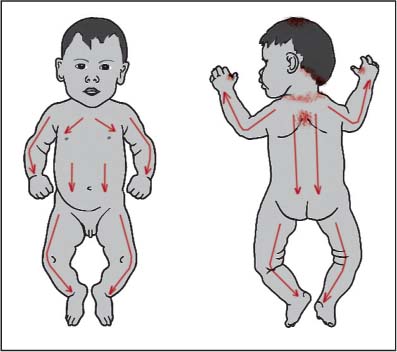
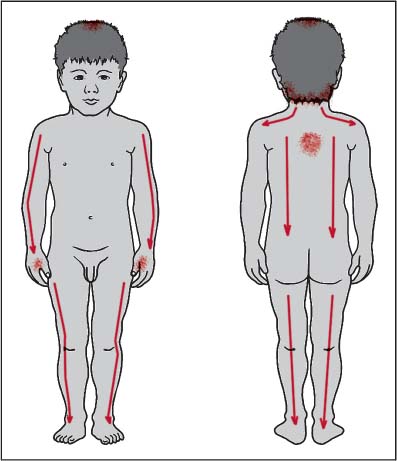
21 Behavioral, Emotional, or Sleep Problems The term “kanmushi” ( This general understanding of kanmushi was more prevalent in shonishin practice before World War II, but since then and partly in response to the needs of modern practice today, such old ideas have generally been restrained. In the modern practice of shonishin we find one surviving offshoot of this concept, the term “kannomushisho” ( As the baby ages, the symptoms can evolve. The irritability, crankiness, crying, screaming, and poor sleep take on various behavioral aspects. It can become part of the communication method of the baby or young child and can be reinforced when the parent responds to address whatever is perceived to have caused the outburst. Such reinforcement as the child ages becomes learned behavior, which can become complicated to deal with. As children start mingling and playing with other children they sometimes play a bit more roughly than other children. They can be very possessive and show tantrums when they do not get what they want, or what has been taken away. In the supermarket such children are capable of really acting up when they cannot get the parent to buy what they see and want. Young children may also show different forms of sleep disturbance such as “night terrors,” bad dreams, waking frequently at night, or sleep walking. Very often the sleep disturbance components leave the parents feeling quite exhausted. All of these behavioral problems are a form of kanmushisho. But depending on the age of the child and the manifestations, they need to be addressed differently. Thus, I will address this issue in three stages. The first stage is the kanmushisho infant. The second is the 2–4-year-old, pre-school child with various manifestations of this, including a really bad “terrible twos.” The third is the older child (school age) where a formal diagnosis of attention deficit hyperactive disorder (ADHD) or hyperactivity has been made. This child may already be on medication to try to control the problems. But the manifestations in the older child are not always ones of hyperactivity. It can include the child who is distracted with poor concentration, so that school grades and participation are poor; here we see diagnoses such as attention deficit disorder (ADD). Main complaints: Since birth, restlessness and irritability; seemed to get easily colicky on bottled milk. He usually woke at 10p.m. screaming and took 2 hours or more to settle down again. All other systems were normal. Assessment: Facial complexion slightly reddish. Otherwise he was a healthy-looking baby. The left pulse was weaker than the right pulse. Diagnosis: Primary liver vacuity pattern. Treatment: Using a teishin, left LR-8 and KI-10 were supplemented. Tapping using a herabari was very lightly applied down the arms, legs, abdomen, back, and neck. Stroking using a silver enshin was very lightly applied down the back and neck. A press-sphere was applied to GV-12. The parents were recommended to change this daily, and if necessary to lightly massage the area around GV-12 when he wouldn’t settle down at night. Second visit—6 days later He was much calmer and more settled following the treatment. He was sleeping fine, was happier, and no longer had the pattern of waking at 10 p.m. and screaming on and off for 2 hours. Treatment: Using a teishin, left LR-8, KI-10, and right LU-9 were supplemented. Tapping using a herabari was very lightly applied down the arms, legs, abdomen, chest, back, and neck. A press-sphere was applied to GV-12. Third visit—2 weeks later He was very good; none of the original symptoms were present. He was very relaxed and calm, smiling a lot. Treatment: Using a teishin, left LR-8, KI-10, and right SP-3 were supplemented. Tapping using a herabari was very lightly applied down the arms, legs, abdomen, chest, back, and neck. A press-sphere was applied to GV-12. The child was discharged from treatment. The parents were instructed to return for treatment if any of the original symptoms recurred. Reflection: I think I was lucky to hit the nail on the head the first time. When we do this, the treatment effects are usually clear and immediate with babies, which is what happened with Noel. I had thought to teach the parents how to do the home treatment on the second visit, but since he had so clearly improved, and what I had done seemed to be enough, I decided not to do this. I did try to get the parents to understand the importance of coming back if there was any recurrence of the symptoms so that we could nip them in the bud. One needs to be careful about dose of treatment until one is sure what the appropriate dose for the child will be. In general, the more the psychological or emotional state of a patient is disturbed, the higher the tendency toward sensitivity; hence be careful of treatment dose. As the child with this kanmushisho tendency becomes older, his or her problems become more complex, with learned behavioral patterns built on top of the kanmushisho tendencies. I have had experiences treating children aged 6–9 years with ADHD who have reacted negatively to the first treatment because I misjudged the dose. It is better to do less and focus on building the treatment relationship at first. It is also advisable when treating a child with behavioral problems not to have the parent bring siblings into the room. Often the child does not want to stay still to receive treatment when a sibling is present. This can be much worse as the children seek to play with each other. It can be very difficult maintaining order and being able to do what you would like when the children are playing in your treatment room. Regulate the qi by moving it downward so as to help calm the child, and treat to restore balance to the channel system so as to help improve overall regulation of qi in the body. Release typical stiff areas that develop in relation to these behavioral problems. Liver vacuity pattern is most commonly treated for this problem. On a baby or small child, where you cannot reliably get information from the pulse and abdomen, select and treat the liver vacuity pattern. To do this, supplement LR-8 and KI-10. An alternative point selection could be to use the fire/ying- spring points LR-2 and KI-2 if the child seems over-heated; he or she would not only be very irritable, crying a lot, and so on, but would have a reddened appearance, almost looking feverish. With older children where you can feel the pulse and abdomen, and can understand what you are feeling, you have the possibility to treat with more discrimination. Liver vacuity pattern is still the more common pattern that shows, but you may find the liver involved in other ways, secondary to lung or spleen vacuity patterns. For example, you may find lung vacuity with liver repletion or lung vacuity pattern with liver vacuity or spleen vacuity pattern with liver repletion, or spleen vacuity pattern with liver vacuity. The method of discriminating repletion or vacuity of the liver is described in Chapter 19, page 132, “Urticaria—Most Likely Pattern-based Root Diagnosis.” In these cases apply treatment as follows: The treatment needs to be applied repeatedly. The kanmushisho pattern is typically part of the constitutional tendencies of the child, and thus symptoms will tend to repeat easily. To counter this, applying treatment regularly for a while is important. Shimizu (1975) mentions applying treatment on average three to five times per month, while Yoneyama and Mori (1964) state it is good to be patient—things improve with regular treatment. To aid consistency and frequency of treatment, it can be very helpful to have the parents apply a short, simplified, light form of the core non-pattern-based root treatment with stroking and tapping at home. This maintains the frequency and pushes the child to respond a little more quickly, which in many cases is very helpful. Chapter 8 describes the application of home treatments. It is important to pay attention to the issues of over-treatment and make sure you check carefully what to do and what you have the parents do at home. For treatment, apply stroking down the arms, legs, back, and abdomen. If the shoulders are stiff, apply stroking across the shoulders. If the neck is stiff, apply stroking down the neck. Apply tapping to around GV-12 (see Fig. 21.1). Additional tapping or stroking can be applied to certain regions and acupoints depending on the severity of the kanmushisho. In general, focus more on the upper back, head, neck, and shoulders. Tapping around GV-12, the GB-20 to BL-10 area, across the occipital region, around GV-20 can be helpful. It can be helpful to start with tapping of the acupoints to which you may need to apply stronger treatment such as needling in later treatment sessions. Check acupoints such as LI-4, LI-2, BL-10, BL-11 for stiffness of the muscles in these regions. Shimizu (1975) makes the following additional recommendations: lightly stroking distally over the webs between the fingers and toes. Apply additional tapping to the following acupoints: LU-5, LI-11, PC-4, ST-36, KI-6. The tapping of these acupoints can be useful as part of the core non-pattern-based treatment if the kanmushisho is strong. If the kanmushisho irritability manifests with abdominal bloating, focus especially on the abdomen, particularly the upper abdomen. Fig. 21.1 Usual stroking plus tapping: • LI-4: 10 to15 times each • GV-12: 20 to 30 times • Shoulder area: 10 to 20 times • Occipital area: 10 to 20 times • GV-20: 10 times For the older child (5 years and older) with kanmushisho- type problems, it is my experience that tapping should be minimized and light stroking should be used. On the baby and young child the combination of stroking and tapping works well. But it seems the tapping can be “stimulating,” which can in some children be an irritant. Thus, on the older child I recommend using stroking applied with slightly more contact and somewhat more slowly. Stroking is applied repetitively down the arms (all yang channels), down the back, down the neck, across the shoulders and down the legs (bladder and stomach channels). For the stroking it can be helpful to use a thicker instrument like the enshin that can warm up with the stroking movements. On subsequent visits, when you are more sure how the child is responding to treatment and what the appropriate dosage needs are, you can start adding other techniques (see Fig. 21.2). If the kanmushisho symptoms are stubborn and do not respond enough to the light stroking and tapping, you may need to increase the dose accordingly on future visits. A simple way of doing this is to insert thin (0.12-mm) needles to acupoints such as LI-4, GB-20/BL-10. For the points of the occipital region you can insert and leave the needles for a short while. For the points on the hands, LI-4, it is usually better to do a quick in and out insertion method. For the older child with, for example, ADHD, it is generally better to use inserted needling methods to the area around GB-20 rather than the usual tapping; if you can retain the needles for a while this is better, otherwise the in and out technique can be used. Needling GV-20 can also be helpful if there is a feeling of sponginess on the point. If the child is older and has ongoing sleeping problems, you may find tightness around the acupoints BL-17. These can be additionally stimulated with in and out needling. Fig. 21.2 Greater number and pressure of stroking plus additional stroking across the shoulders. Light tapping around: • LI-4 • GV-12 • Occipital area • GV-20 area Leaving a press-sphere on GV-12 is generally helpful. Sometimes one also finds knots on toddlers and older children around BL-15. Leaving press-spheres on these can also be helpful. For sleep disturbance, leaving press-spheres on BL-17 is good. For the older child or those who can deal with a higher dose of treatment you can leave press-tack needles on the bladder channel acupoints. In some children the shoulders are very stiff, and there is a strong knot around, for example, GB-21; leaving press-spheres on these can be useful. Sometimes, to help the child with liver weak constitution tendencies and behavioral or sleep problems, leaving press-spheres on related back shu points can be helpful. In a liver vacuity pattern we treat the liver and kidney channels, thus we leave press-spheres on BL-18 on one side and BL-23 on the other side of the back. Mike Smith recommends leaving a press-sphere to the extra point behind shen men on the ear (Smith, personal communication). He recommends this for children with ADD and ADHD. I have found it useful in a general way to help calm the child. Okyu is used if the symptoms are more stubborn, and not responding sufficiently to treatment. GV-12 is a main treatment point. Manaka recommends it for severe crying at night in the infant (Manaka, Itaya, and Birch 1995). Shiroda (1986) recommends it with GV-4 for the very agitated “fretful” child. If there are strong reactions around BL-17 and BL-18, and treatment of those reactions with needling, press-spheres, or press-tack needles has not changed them much, and the symptoms have improved little, okyu can be applied on these points; be careful not to let it become too hot, the 80% cone moxa approach is better—put the moxa out as soon as a little heat is felt (see Chapter 13). In general, the use of cupping on kanmushisho children is not talked about much. If the shoulders and interscapular regions are very stiff, light, low-dose cupping can be applied carefully on the shoulders and thoracic spine to try to help release the tension there. This, like moxa, is not a first or second line of treatment for children with kanmushisho, but can be used as an alternative back-up strategy if other approaches have not been so helpful. Shimizu (1975) recommends the use of bloodletting of jing points in more severe cases of kanmushisho. The most common points treated are LI-1, SI-1, and less often LR-1. Yoneyama and Mori (1964) also state that on occasion in stubborn, more severe cases one needs to apply some blood-letting; they recommend bloodletting LI-2. Shimizu (1975) also mentions a condition he calls “mushi fever.” This refers not to the feverish child, but the “over-heated” child who has been too active. For this, as well as recommending light tapping only on the head, shoulders, and upper back to help with cooling the child down, he mentions that bloodletting of LI-1 and/or SI-1 may be needed. Obviously one would prefer not to have to do bloodletting as it can be difficult to do on children, but if your technique is good, it should not be too problematic. It is very important that you have a painless technique. Generally speaking it is better and easier if you do not do this on a child until you have practiced the technique described in Chapter 15, and can do it painlessly on demand. It should come as no surprise that sugar intake should be discussed with the parents, as should intake of soft drinks like Coca-Cola. It is surprising how unaware some parents are of the inappropriateness of allowing their overactive child to drink caffeine-rich drinks such as sugared Coca-Cola. These behavioral problems can also be triggered or irritated by consumption of cow’s milk products, thus it may be necessary to instruct parents on how to test for and eliminate them from the diet of their child. When there are behavioral problems with a child, there is often tension in the family environment as the parents become stressed and irritated by the child’s behavior. This is one area where the application of a light form of the shonishin treatment as home treatment can be very helpful. Not only does the child benefit directly from having the treatment applied regularly rather than just when they come to your clinic, but it helps the parents. In some cases it not only helps the parents feel less frustrated as they start to feel they can do something to help, but the light, friendly actions of the treatment coupled with all the soft tactile stimulation help restore a less stressed relationship and bond between parent and child. For the child with sleep problems I recommend making sure that the treatment is done before going to bed at night. For the child with behavioral manifestations of the kanmushisho—angry, irritable, cries, shouts a lot—have the parent use only stroking down the arms, legs, and back. My colleague Diana Pinheiro from Lisbon describes her experience that this stroking applied with a spoon can be very helpful to calm the patient down. She feels that as the spoon warms up with the stroking, the child becomes “cooler” (Pinheiro, personal communication). Here you can try having the parent apply the stroking slowly with very slightly more pressure to encourage these kinds of changes. The following case is from my colleague, Zoe Brenner of Bethesda, Maryland in the United States. Case 2 Main complaints: Colin was 6 weeks old when I first saw him. He was screaming constantly. The problem was diagnosed as severe colic. His mother reported that he screamed pretty much around the clock. He was obviously terribly distressed and so were his parents. He was breast-fed and his mother was on a very restricted diet. They had tried hypoallergenic formula and small doses of anti-acid medication, but this did not help and he was still quite distressed. Treatment: A very general and quick treatment using small strokes with an enshin was applied. Treatment was applied by stroking down his legs on the outside, up the inside, down his arms front and back; clockwise around his belly and down the center area of the chest. When the stroking was applied down his back, he calmed down noticeably. Treatment was finished very quickly. After discussing with his mother his condition and scheduling, he stopped crying. It was decided to have him come back three times that week for these quick treatments. Second visit—next day His mother reported that he had been quieter and better for about 4 hours after the first treatment. Treatment: Given his response the day before, treatment was started on his back. As the enshin was lightly stroked down his back he immediately stopped crying. Stroking was then applied down his arms, clockwise on his belly, down the lateral aspects of his legs and up the medial aspect of his legs. After this he had calmed down enough for his pulses to be read. His lung and spleen pulses were the weakest (lung vacuity pattern), so very light stroking was applied over LU-9 on the left wrist and the pulse was checked again. There was enough change. His color improved from a darker reddish hue to a lighter shade. Third visit—2 days later When Colin came into the outer part of the office he calmed down. His mother said that he had been generally much better. It was easier to console him but he still had some difficulties, especially at night. Treatment: The treatment from the second visit was repeated with the addition of very light stroking of SP-3. Fourth visit—4 days later His mother reported that he had generally been much happier and was showing signs of being more “normal,” smiling and being playful rather than constantly in distress. Treatment: Same as the previous visit with the addition of draining the stomach channel: stroking a little more heavily against the flow of the stomach channel over right ST-40. Fifth visit—2 days later His mother reported that she was so relieved that he was showing such signs of improvement. He had even stopped fussing when they were on the way to my office. Before, he would scream pretty much around the clock and was now having good periods of relief each day. Treatment: Same treatment as on the last visit. Treatment continued like this, with him coming in on average twice a week for a while. He had some rough days but generally better periods. When the family went away for 10 days, he had more symptoms again after 6 days, so it seemed he was still reactive. His mother was taught to apply some gentle stroking while they were away but that had not worked much. So the treatment schedule of three treatments that first week was tried. The next week two treatments were given. Gradually, treatments were worked down to one treatment a week while maintaining the improvements. Colin’s mother was quite worried that when they went home to Europe for the summer he might regress. But he was doing well when they left and while away he had done extremely well with almost no symptoms. He was 4.5 months old when they left for the summer and so his digestion was getting stronger while he was away and he didn’t need treatment when they returned. We arranged that they would call if further treatment was needed.
Kanmushisho—the Cranky Child
 ) refers to concepts in the historical development of pediatric medicine in Japan. It came to have a very broad meaning. Shimizu (1975) lists the following symptoms or manifestations as associated with kanmushi: insomnia, night crying, night terror, bad mood, irritability, cries a lot, convulsions, biting people, biting nails, abdominal bloating due to over-eating, temporary fever, vomiting milk, vomiting in general, poor appetite, diarrhea, runny nose, stuffy nose, sore throat, cough, easily catches cold, allotriophagy (desire for unusual or abnormal food), excessive drooling, tics, urticaria, swollen lymph glands. When the condition is strong one can see other manifestations of the condition such as: a bluish tinge to the white of the eyes, blue vein apparent between the eyes, stiff and angry facial expression, the appearance of the hair of the head standing up (Shimizu 1975). One can see that it covers many conditions for which parents might bring their child for treatment. Shimizu is of the opinion that in general kanmushi is to do with a kind of over-sensitivity of the child to various stimuli (environ-mental, nutritional, emotional, etc.) and is both partly related to stages of development of the child and an underlying constitutional type weakness in the child, which predisposes them to these over-sensitivities (Shimizu 1975).
) refers to concepts in the historical development of pediatric medicine in Japan. It came to have a very broad meaning. Shimizu (1975) lists the following symptoms or manifestations as associated with kanmushi: insomnia, night crying, night terror, bad mood, irritability, cries a lot, convulsions, biting people, biting nails, abdominal bloating due to over-eating, temporary fever, vomiting milk, vomiting in general, poor appetite, diarrhea, runny nose, stuffy nose, sore throat, cough, easily catches cold, allotriophagy (desire for unusual or abnormal food), excessive drooling, tics, urticaria, swollen lymph glands. When the condition is strong one can see other manifestations of the condition such as: a bluish tinge to the white of the eyes, blue vein apparent between the eyes, stiff and angry facial expression, the appearance of the hair of the head standing up (Shimizu 1975). One can see that it covers many conditions for which parents might bring their child for treatment. Shimizu is of the opinion that in general kanmushi is to do with a kind of over-sensitivity of the child to various stimuli (environ-mental, nutritional, emotional, etc.) and is both partly related to stages of development of the child and an underlying constitutional type weakness in the child, which predisposes them to these over-sensitivities (Shimizu 1975).
 ). Kannomushisho or “kanmushisho” (
). Kannomushisho or “kanmushisho” ( ) is used in a more limited way to refer to the infant who will not settle down, is distressed, cries and screams a lot, sleeps badly, is irritable, and so on. In Western countries it is common to hear newborns described as being “colicky.” In many cases it may involve the baby being “colicky” and what the baby is fed may need to be examined, but many cases are probably not due to being colicky; rather, there are other issues. Following the traditional theories and models of acupuncture practice that can be found in Keiraku Chiryo or Meridian Therapy, we can say that these are principally signs of disturbance of the liver channel. The constitutionally liver weak child can show this tendency, such behavioral problems being a hallmark of that type. But the presence of a symptom associated with a particular channel, here the liver channel, does not necessarily indicate what the state of that channel is; it could be weak or replete. Generally, when a young baby presents with these symptoms, we treat it as a liver vacuity pattern. When an older baby or young child presents for treatment with these behavioral problems, if we are able to access the radial pulse clearly, we sometimes find that the child has liver repletion, which means we apply draining technique to the liver channel. But this is difficult to determine if we cannot access the radial pulses clearly. The general non-pattern-based root treatment is very helpful for this kind of baby or child. When in addition the liver channel disturbance is addressed, it seems to work very well.
) is used in a more limited way to refer to the infant who will not settle down, is distressed, cries and screams a lot, sleeps badly, is irritable, and so on. In Western countries it is common to hear newborns described as being “colicky.” In many cases it may involve the baby being “colicky” and what the baby is fed may need to be examined, but many cases are probably not due to being colicky; rather, there are other issues. Following the traditional theories and models of acupuncture practice that can be found in Keiraku Chiryo or Meridian Therapy, we can say that these are principally signs of disturbance of the liver channel. The constitutionally liver weak child can show this tendency, such behavioral problems being a hallmark of that type. But the presence of a symptom associated with a particular channel, here the liver channel, does not necessarily indicate what the state of that channel is; it could be weak or replete. Generally, when a young baby presents with these symptoms, we treat it as a liver vacuity pattern. When an older baby or young child presents for treatment with these behavioral problems, if we are able to access the radial pulse clearly, we sometimes find that the child has liver repletion, which means we apply draining technique to the liver channel. But this is difficult to determine if we cannot access the radial pulses clearly. The general non-pattern-based root treatment is very helpful for this kind of baby or child. When in addition the liver channel disturbance is addressed, it seems to work very well.
 General Approach for the Cranky, Irritable Child
General Approach for the Cranky, Irritable Child
 Goals of Treatment
Goals of Treatment
 Most Likely Pattern-based Root Diagnosis
Most Likely Pattern-based Root Diagnosis
 For lung vacuity with liver repletion pattern: supplement LU-9, SP-3, or LU-5, SP-9 on one side and drain LR-3 or LR-8 on the other side of the body.
For lung vacuity with liver repletion pattern: supplement LU-9, SP-3, or LU-5, SP-9 on one side and drain LR-3 or LR-8 on the other side of the body.
 For the lung vacuity, liver vacuity pattern: supplement LU-9, SP-3, or LU-5, SP-9 on one side and LR-3 or LR-8 on the other side of the body.
For the lung vacuity, liver vacuity pattern: supplement LU-9, SP-3, or LU-5, SP-9 on one side and LR-3 or LR-8 on the other side of the body.
 For the spleen vacuity with liver repletion pattern: supplement SP-3, PC-7, or SP-9, PC-3 on one side and drain LR-3 or LR-8 on the other side of the body.
For the spleen vacuity with liver repletion pattern: supplement SP-3, PC-7, or SP-9, PC-3 on one side and drain LR-3 or LR-8 on the other side of the body.
 For the spleen vacuity with liver vacuity pattern: supplement SP-3, PC-7, or SP-9, PC-3 on one side and LR-3 or LR-8 on the other side of the body.
For the spleen vacuity with liver vacuity pattern: supplement SP-3, PC-7, or SP-9, PC-3 on one side and LR-3 or LR-8 on the other side of the body.
 Typical Non-pattern-based Root Treatment
Typical Non-pattern-based Root Treatment
 Recommendations for Symptomatic Treatment
Recommendations for Symptomatic Treatment
Needling
Press-spheres (Ryu), Press-tack Needles (Empishin), and Intra-dermal Needles (Hinaishin)
Okyu—Direct Moxa
Cupping
Bloodletting
 Other Considerations
Other Considerations
Dietary
Home Treatment
 Further Case Histories
Further Case Histories
Colin, Boy Age 6 Weeks
Behavioral, Emotional, or Sleep Problems
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree