Fig. 3.1
Plain radiograph of the knee demonstrating an aggressive appearing lesion in the distal femur. Note the bone destruction, osteoid formation, and periosteal reaction
3.3 Types of Biopsy
After the initial workup is complete, the physician must decide whether to proceed with biopsy for tissue diagnosis. Only lesions that are definitively benign based on physical exam or imaging characteristics can avoid biopsy. All other lesions, or lesions in which the diagnosis is unclear should undergo tissue sampling. Adequate pre-operative imaging is crucial to formulate proper differential and biopsy approach. The imaging should not be older than 4–6 weeks as malignant tumors can rapidly grow. Once the decision to proceed with biopsy has been made, there are several potential methods that can be employed to obtain the tissue. Before the biopsy is performed, the definitive resection should be considered to allow proper placement of the biopsy tract. If the performing surgeon is not comfortable with the definitive surgical resection, then they should not perform the biopsy and should refer the patient to a specialized center (Springfield and Rosenberg 1996). The main consideration is to use the technique that will provide the highest diagnostic accuracy while minimizing complications. Choices of biopsy method include: fine needle aspiration (FNA), core needle biopsy, open incisional biopsy, and excisional biopsy.
3.3.1 Fine Needle Aspiration
Fine needle aspirations typically use 22- to 25-gauge needles and several passes are made into the periphery of the tumor. There are several distinct advantages of fine needle aspiration over other biopsy methods. It is less costly, can be performed in the office without anesthetic, and an immediate answer can be secured during the patient’s office visit (Kaffenberger et al. 2010). Image guidance is not needed for FNA of palpable lesions that are safely away from vital underlying structures such as blood vessels but non-palpable lesions are better biopsied with image guidance. Either an ultrasound or a CT scanner can be used as the imaging modality of choice depending upon the expertise of the physician performing the biopsy. The main limitation of the fine needle aspiration is that it does not provide the evaluation of the tissue architecture (Fig. 3.2). A recently published study reported a diagnostic sensitivity and specificity of 89 % with fine needle aspiration (Ng et al. 2010). Other manuscripts have presented lower success rates with 79 % sensitivity and 72 % specificity (Kasraeian et al. 2010). These two studies demonstrate the most important rate-limiting step involved with the accuracy of FNA biopsy for musculoskeletal tumors, an expert cytopathologist. If there is no well-trained cytopathologist within the institution, utilization of fine needle aspiration biopsy is not a realistic option for diagnosis.
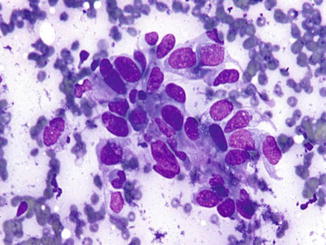
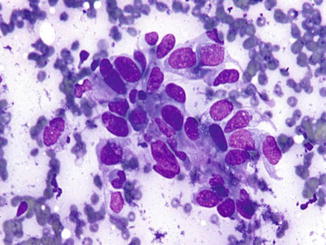
Fig. 3.2
Example of sample obtained from fine needle aspiration (FNA). The office-based biopsy yields a small sample of cells
3.3.2 Core Needle
A second type of needle biopsy, called core needle biopsy, is slightly more invasive than a fine needle aspiration but can still be performed in the office without the need for surgical intervention (Adams et al. 2010). A 14-gauge needle is utilized. In this technique a local anesthetic is necessary. This additional needlestick minimally increases the risk of complication such as an allergic reaction. The costs of a core needle biopsy is slightly higher than FNA secondary to increased tissue handling needs that are required for its successful completion, but still much less than an open biopsy (Skrzynski et al. 1996). This biopsy technique can be performed either with or without image guidance depending upon the presence of a non-palpable or palpable mass. A recently published paper has also documented the sensitivity and specificity of this technique at 79 % and 82 % respectively (Kasraeian et al. 2010). Based on these success rates, a trained musculoskeletal pathologist, rather than a cytologist, is a minimum requirement and there is an additional cadre of pathologists that have been required to have the expertise to evaluate this type of specimen (Heslin et al. 1997).
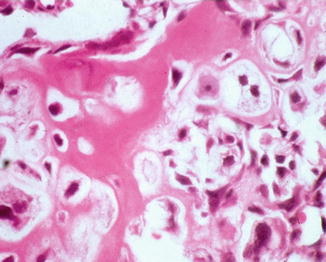
3.3.3 Open Surgical Biopsy
Open biopsy is the gold standard technique as a study when diagnostic tissue for a bone lesion is required (Kasraeian et al. 2010). This procedure provides additional volume of the available specimen as well as a generally higher sensitivity and specificity with respect to diagnosis (Fig. 3.3). A representative sample is taken through the smallest possible longitudinal incision. It does have some downsides though; the risk of infection is higher, the cost is higher, and the risk of bleeding complications is increased. Additional bleeding within the wound bed can cause the possibility of further contamination by malignant cells. Any resultant hematoma should be considered contaminated and must be resected with the eventual definitive procedure. In addition, an open biopsy must be performed in an operating room using strict aseptic technique. The use of an operating room has additional costs as well. There are two types of open biopsy that can be performed. An excisional biopsy is performed by removing the entire tumor. An incisional biopsy removes a portion of the tumor to obtain diagnosis, and is the most common biopsy used for the diagnosis of bone sarcomas. It can be combined with frozen section analysis to ensure that diagnostic tissue has been obtained. It is generally accepted that the extraosseous component of the tumor is representative of the diagnosis and is adequate. Sampling of the intraosseous portion requires violation of the bone cortex and may pre-dispose the patient to pathologic fracture. This should only be done if there is no extraosseous portion. If the intraosseous portion requires sampling, the smallest corticotomy needed to gain diagnosis should be used.