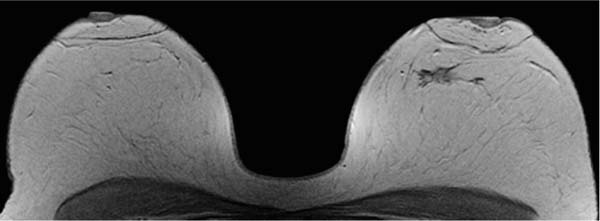
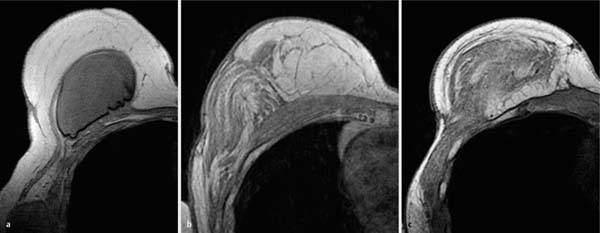
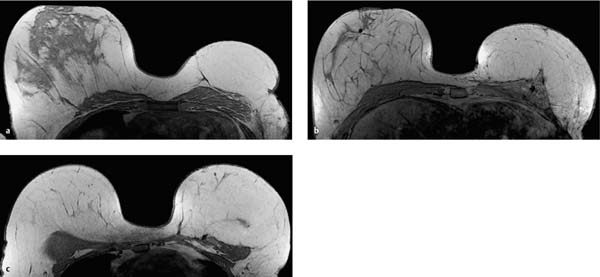
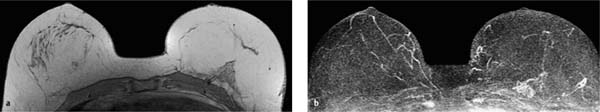
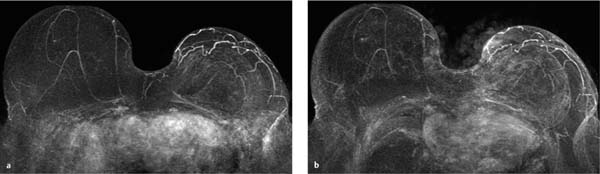
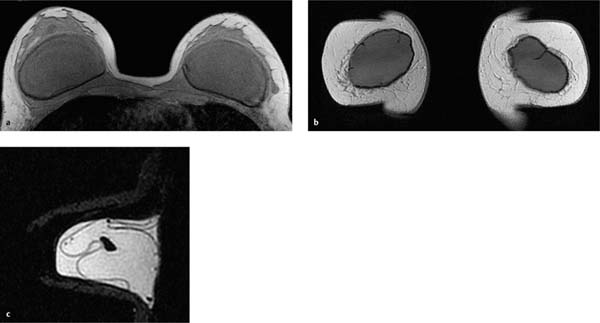
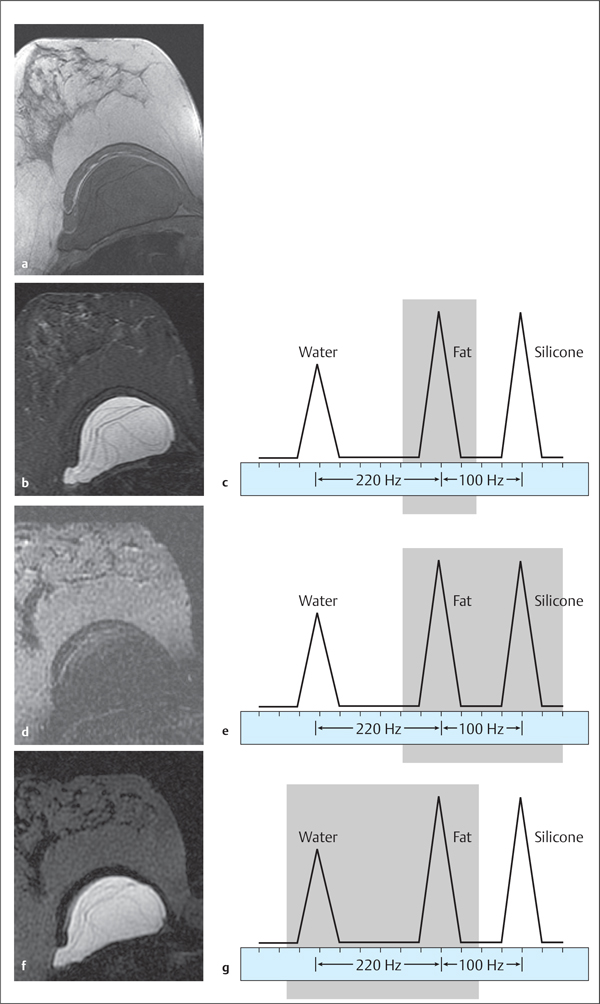
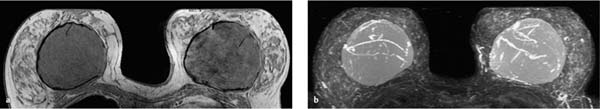
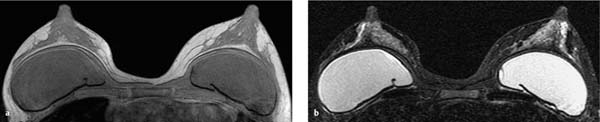
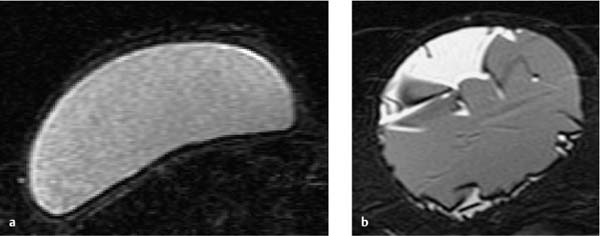
14 Autologous and Prosthetic Breast Reconstruction In general, breast plastic surgery techniques are performed for breast size reduction (Fig. 14.1), breast augmentation, and breast reconstruction. Reconstruction of the female breast can be performed using autologous tissue or prosthetic material, both of which are discussed here separately. Breast MRI images after flap reconstruction are dependent upon the technique and type of donor tissue used. The most commonly used techniques are the latissimus dorsi myocutaneous flap technique (Fig. 14.2) and the thoracoepigastric flap technique, which typically leave the donor tissue connected to the original blood supply (pedicled flap). The pedicle can either be ipsilateral to the reconstructed breast, with the pedicle leading to the reconstructed area from the caudal aspect (Fig. 14.4), or contralateral to the reconstructed breast, with the pedicle leading to the reconstructed area from the mediocaudal aspect. The most commonly used technique for autologous breast reconstruction is the TRAM (transverse rectus abdominis myocutaneous) flap technique (Fig. 14.3). In addition, there are other flaps that can be used for breast reconstruction (e.g., contralateral superior rectus flap, vertical rectus flap, gluteal flaps). Fig. 14.1 Reduction mammaplasty with periareolar incision. T1w precontrast image shows retromamillary scar after periareolar incision. Fig. 14.2a–c Different forms of latissimus dorsi flaps. a T1w precontrast slice image: latissimus dorsi flap combined with breast implant. b T1w precontrast slice image: latissimus dorsi flap for reconstruction of lateral breast aspect. c T1w precontrast slice image: latissimus dorsi flap for reconstruction of entire breast. a T1w precontrast slice image: predominantly lipomatous flap. b T1w precontrast slice image: TRAM flap with pedicle near the thoracic wall. c T1w precontrast slice image: fasciocutaneous TRAM flap. Fig. 14.4a, b TRAM flap pedicle. a T1w precontrast slice image: typical TRAM flap for reconstruction of the left breast with pedicle near the thoracic wall. b Subtraction MIP. Examinations performed for the purpose of detecting and evaluating complications of prostheses are fundamentally different from those performed to rule out malignancy (Fig. 14.5). First, no dynamic study is performed in such an examination, dispensing with the need for intravenous administration of contrast material. Second, special sequences are employed to selectively evaluate the different prosthesis components (e.g., silicone, water). Orientation. In contrast to the dynamic breast MRI examination, it is obligatory in the examination of a woman with breast prostheses to use several orientations (Fig. 14.6). In addition to the customary axial slice orientation, images with sagittal orientation have proven advantageous for the detection of extramammary silicone accumulations, especially cranially and caudally to the prosthesis, as well as prosthesis deformations in the craniocaudal direction. Thin slices (2 mm) should be attained to detect subtle changes (see gel bleeding, p. 207). IR sequences. The relative resonant frequencies of fat and silicone differ only slightly. Silicone has a resonant frequency ~100 Hz lower than that of fat, and ~320 Hz lower than that of water (Fig. 14.7c, e, g). The most effective sequences for differentiating the different fluid components of a prosthesis are the inversion recovery (IR) sequences with fat suppression (Fig. 14.7b, d, f). Using such IR sequences with additional suppression of the water signal allows the signal-intense depiction of silicone, while suppressing the signal of the saline component and the surrounding fat tissue (Fig. 14.7f). On the other hand, IR sequences performed with the additional suppression of the silicone signal allow the selective depiction of the saline component. In this way it is possible to image both lumina of a double-lumen prosthetic implant separately (silicone/saline). In addition, fluid accumulations between the prosthesis shell and the capsule of single-lumen implants can also be more easily detected using such protocols. Fig. 14.5a, b Diagnostic MRI in patient with breast prosthesis: with and without swapped phase-encoding gradient. a Subtraction MIP with mediolateral phase-encoding gradient. b Subtraction MIP with ventrodorsal phase-encoding gradient. Fig. 14.6a–c Diagnostic MRI in patients with breast prosthesis: different orientations. a Axial orientation. b Coronal orientation. c Sagittal orientation. a Standard MRI with usual T1w precontrast images. b IR T2w examination with signal-intense depiction of water and silicone, and suppression of the fat signal. Signal-intense areas within prosthesis and parenchyma. c Schematic diagram of fat suppression. d Silicone-suppressed IR examination with fat suppression. e Schematic diagram of fat and silicone suppression. f Water-suppressed IR examination with fat suppression. Only silicone is depicted with high signal intensity. g Schematic diagram of fat and water suppression. SE sequences. Other measurement sequences used for the imaging of breast prostheses include fast SE sequences, with and without water-signal suppression. These sequences, however, do not allow such selective imaging of the prosthesis silicone component as can be achieved with the IR sequences described above. Position. Breast prostheses can be surgically implanted ventral to the pectoralis major muscle (prepectoral/subglandular position, Fig. 14.8), or dorsal to it (subpectoral position, Fig. 14.9). Shape. A breast implant is typically oval in shape, or rarely round. Deformation of the surface is not a pathological finding as long as the outer shell is intact. The outer surface of the implant shell is smooth or textured. It is usually made of silicone elastomers and there is typically a reactive formation of a thin surrounding fibrous capsule after surgical implantation. Silicone found outside this capsule is pathological. Because of the limited scope of this atlas, it is not possible to give detailed information on the great variety of implants available on the market; for such information the reader is referred to specialist literature on the subject. The following discourse is therefore confined to the materials most often used: saline and silicone. Single- and double-lumen prostheses. When evaluating the internal structures of an implant, it is necessary to differentiate between single-lumen and double-lumen implants. The singlelumen prosthesis consists of a single chamber typically filled with a viscous silicone gel (Fig. 14.10a) or (increasingly) a saline solution. The double-lumen prosthesis consists of an inner chamber typically filled with a viscous silicone gel, and an outer chamber containing saline (Fig. 14.10b). A modification of this prosthesis in which the inner chamber contains saline and the outer chamber contains silicone is referred to as a “reverse double-lumen.” Fig. 14.8a, b Prepectoral/subglandular prostheses. a T1w precontrast slice image: prostheses implanted ventral to the pectoral muscle. b IR T2w MIP. Fig. 14.9a, b Subpectoral prostheses. a T1w precontrast slice image: prostheses implanted dorsal to the pectoral muscle. b IR T2w slice image.
Diagnostic MRI after Autologous Breast Reconstruction
Diagnostic MRI of Breast Prostheses
Normal Findings
 The prosthesis shell is the silicone elastomer casing surrounding the prosthesis contents (a part of the prosthesis). The shell must be differentiated from the collagen tissue capsule (scar tissue) that is formed around the breast implant as a reactive process after implantation.
The prosthesis shell is the silicone elastomer casing surrounding the prosthesis contents (a part of the prosthesis). The shell must be differentiated from the collagen tissue capsule (scar tissue) that is formed around the breast implant as a reactive process after implantation.
< div class='tao-gold-member'>
Autologous and Prosthetic Breast Reconstruction
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree