38 Asthma
Etiology and Pathogenesis
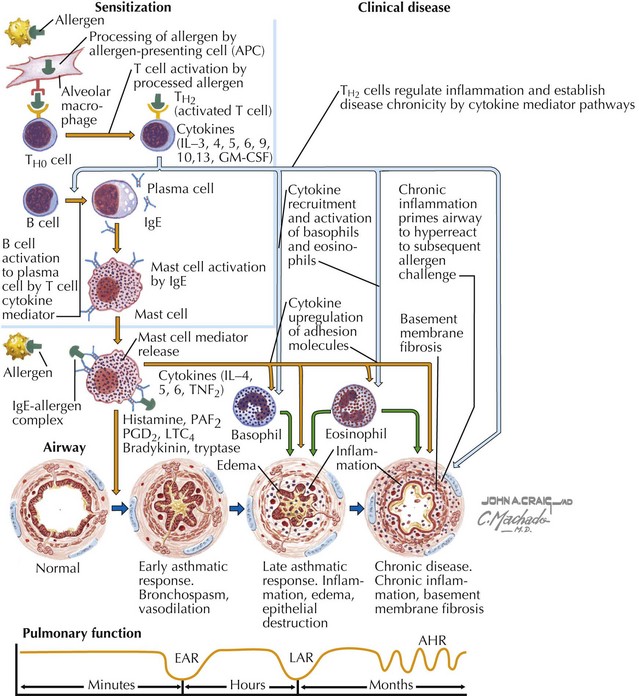
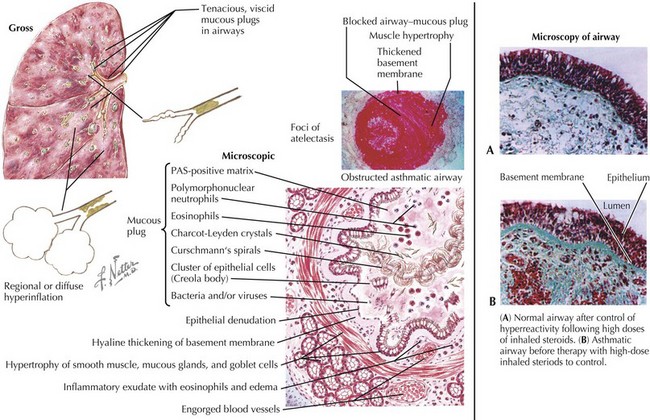
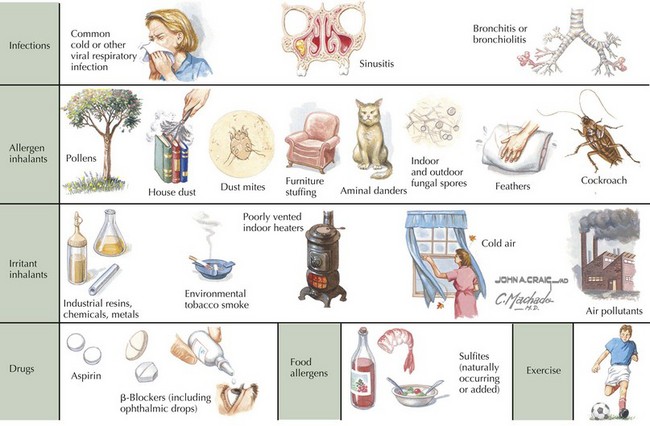
Asthma is characterized by the presence of three airway components: inflammation, obstruction, and hyperresponsiveness. Chronic airway inflammation establishes baseline airway edema and obstruction, which sets the stage for acute exacerbations. During acute exacerbations, inciting triggers (Box 38-1) cause inflammation and bronchoconstriction of already hyperresponsive airways. Key cellular components involved in the pathogenesis of asthma include mast cells; eosinophils; and, to some degree, neutrophils, T cells, macrophages, and epithelial cells (Figures 38-1 and 38-2).
Clinical Presentation
A patient or family history of allergy and atopic skin disease may be present. It is important to inquire about the setting(s) in which symptoms occur because a variety of inciting triggers exist (Box 38-1 and Figure 38-3). A patient should also be assessed for comorbid medical conditions, including GER, allergic rhinitis, sinusitis, and obesity, all of which can exacerbate asthma symptoms. For a patient with a previous asthma diagnosis, it is useful to inquire about the frequency of ED visits and hospital admissions, oral steroid use, and any history of severe complications (e.g., endotracheal intubation or admission to the intensive care unit [ICU]).
Differential Diagnosis
If considering a diagnosis of asthma, the time-worn axiom must be remembered that “all that wheezes is not asthma.” Before a diagnosis of asthma can be confirmed, alternative diagnoses must be considered (Table 38-1). Furthermore, not all wheezes are equal. For example, monophonic wheezing associated with foreign body aspiration is distinct from polyphonic wheezing associated with asthma.
Table 38-1 Differential Diagnosis of Asthma in Children
| Differential Diagnosis | Suggested Confirmatory Tests | |
|---|---|---|
| Upper airway diseases | Allergic rhinitis or sinusitis | Physical examination, sinus CT scan |
| Obstruction of large airways | Foreign body in trachea or bronchus Vocal cord dysfunction Vascular rings or laryngeal webs Tracheomalacia Tracheal- or bronchostenosis Enlarged lymph nodes or tumor | Chest radiography Laryngoscopy Barium swallow, chest MRI Laryngoscopy, flexible bronchoscopy Chest radiography, chest CT scan, bronchoscopy Chest radiography, chest CT scan |
| Obstruction of small airways | Viral bronchiolitis Bronchiolitis obliterans Cystic fibrosis Bronchopulmonary dysplasia Heart disease | History, chest radiography, viral antigen or PCR testing Chest CT scan, lung biopsy Chest radiograph, sweat chloride test, genetic test Prenatal history, chest radiography, chest CT scan Chest radiograph, ECG, echocardiography |
| Other causes | Gastroesophageal reflux Oromotor dysfunction leading to chronic aspiration Pulmonary edema Tracheoesophageal fistula | pH probe, barium swallow, nuclear milk scan Modified barium swallow, speech pathology evaluation Chest radiography Chest radiography, fluoroscopy, chest CT |
CT, computed tomography; ECG, electrocardiography; MRI, magnetic resonance imaging; PCR, polymerase chain reaction.
Adapted from the Expert Panel Report 3 (EPR3): Guidelines for the Diagnosis and Management of Asthma. Washington, DC, U.S. Department of Health and Human Resources, 2007, p 12. Available at http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm.