CHAPTER 22 Assisted reproduction treatments
Introduction
Since the first successful birth following IVF in 1978, there have been considerable advances in the field of ART and more than 3 million babies have been born across the world. ART is now widely available, and in a single year (2004), more than 360,000 treatment cycles were carried out in Europe. In the UK, a total of 44,275 IVF/micromanipulation and frozen embryo replacement (FER) cycles were reported in 2006, resulting in 12,596 livebirth events (Human Fertilisation and Embryology Authority 2008). The number of conventional IVF cycles remained reasonably steady between 1998 and 2008, while the number of ICSI treatment cycles has been increasing steadily since its introduction (Figure 22.1) Human Fertilisation and Embryology Authority 2008).
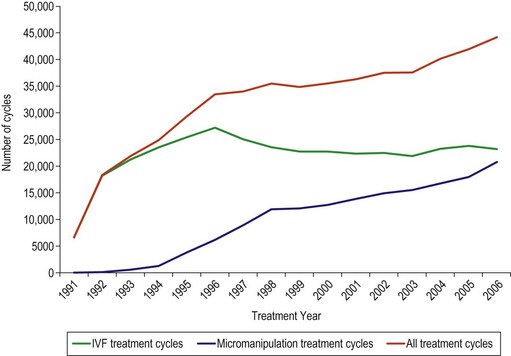
Figure 22.1 Number of treatment cycles 1991–2006.
Source: Human Fertilisation and Embryology Authority (2008).
The Human Fertilisation and Embryology Authority (HFEA) was established in 1991 by the Human Fertilisation and Embryology Act 1990 to regulate and inspect all UK clinics providing ART, and was the first statutory body of its kind in the world. The introduction of guidelines into clinical practice in general and in assisted reproduction in particular has led to an ever-increasing role for an evidence-based approach to the provision of these services. Clinical guidelines for the assessment and treatment of people with fertility problems have been published by the National Institute for Clinical Excellence (2004) to streamline services and avoid unnecessary waste of resources. This chapter will review the current status of conventional IVF, ICSI and other treatments, new developments in ART and the clinical risks associated with these techniques. The obstetric and neonatal consequences of these treatments and, in particular, the impact of the number of embryos transferred on the outcome will be discussed.
Selection and Evaluation of Patients
Although IVF was initially introduced to bypass tubal blockage, the currently available techniques enable the treatment of various causes of infertility. The current indications are shown in Box 22.1.
Evaluation of pelvis
The diagnosis of PCOS is currently based on the definition derived by the Rotterdam Consensus Workshop, which suggested the presence of 12 or more follicles measuring 2–9 mm in diameter and/or an ovarian volume of more than 10 cm3 for the ultrasound diagnosis (Balen et al 2003). Stromal vascularity and blood flow velocities are higher in women with polycystic ovaries (Agrawal et al 1998), and this may account for their tendency towards ovarian hyperstimulation in response to gonadotrophin therapy.
Endometriosis has been shown to have a negative effect on the outcome of ART, with affected women demonstrating a reduced response to ovarian stimulation (Gupta et al 2006); however, reports on its effects on embryo quality and implantation potential are conflicting. Moderate and severe degrees of endometriosis, often characterized by rectovaginal disease and the presence of ovarian endometrioma, can usually be diagnosed by transvaginal ultrasound (Moore et al 2002).
The presence of a hydrosalpinx is associated with poor implantation and pregnancy rates, and early pregnancy loss. The exact mechanism is unknown but substances toxic to the endometrium are thought to be produced that have a negative effect on endometrial receptivity (Strandell 2007). Salpingectomy, ideally performed laparoscopically, prior to IVF has been shown to be beneficial and is recommended. The diagnosis of hydrosalpinx can generally be made using transvaginal ultrasound with a high degree of confidence.
Ultrasound assessment of the uterus is generally restricted to measurement of the endometrial thickness and a description of the locality and size of any fibroids. Conventional ultrasound may also detect uterine anomalies, although these are more readily identified and correctly qualified with three-dimensional ultrasound. The diagnosis of uterine anomalies is important as they are associated with lower implantation rates and increased rates of early miscarriage, preterm labour and malpresentations (Lin 2004). The outcome appears to relate more to the length of the remaining uterine cavity than the degree of septum, and this may be measured reliably with three-dimensional ultrasound (Salim et al 2003).
The diagnosis and classification of fibroids into subserosal, intramural and submucosal is usually straightforward, and this is important as these have a progressively negative effect on pregnancy rates. Whilst intramural fibroids measuring more than 4 cm in diameter and submucous fibroids of any size are thought to have a negative effect on the outcome of fertility treatment and to be associated with lower pregnancy rates, the effect of smaller intramural fibroids on reproductive outcome is unclear (Oliveira et al 2004). There is also doubt about the exact impact of endometrial polyps, the other commonly encountered intrauterine pathology, on treatment outcome and early pregnancy. Some authors suggest conservative management, especially if the polyp is small (Isikoglu et al 2006), but this can be difficult in patients undergoing fertility treatment or with a history of miscarriage when a polyp is identified before treatment begins. Polyps are usually evident with conventional transvaginal imaging, although false-positive diagnoses are common. Saline infusion sonohysterography can reduce this and facilitate appropriate operative planning (Bartkowiak et al 2006). Delineation of the polyp with saline ensures that the size and position of the polyp can be defined accurately, allowing surgeons to modify their approach and resect the larger, more broad-based polyps rather than planning for simple polypectomy. Hysteroscopy is the gold standard technique for uterine cavity assessment, and may be necessary if diagnosis of intrauterine pathologies is in doubt.
Assessment of ovarian reserve
Evaluation of ovarian reserve has become an integral part of the pretreatment assessment of a woman about to undergo ART, and is recommended for all women planning ART (Speroff and Fritz 2005). The aim is to identify women likely to respond poorly, those who have a low chance of success and who are more likely to have their treatment cycle cancelled, and those prone to ovarian hyperstimulation which is associated with significant morbidity and even mortality. Accurate assessment of ovarian reserve and prediction of response therefore facilitates pretreatment counselling of couples of their potential risks, and allows treatment to be tailored to the individual, potentially increasing the number of oocytes retrieved without risking an exaggerated response. Ovarian reserve, defined by the size and quality of the remaining ovarian follicular pool at any given time, reflects the fertility potential of a woman (Broekmans et al 2006).
Although women’s age is an important predictor of ovarian reserve and response, a great deal of interindividual variation exists, even among women of the same age (te Velde and Pearson 2002). This is indicative of a wide variation in the rate of age-related decline in the ovarian follicle population. Several endocrine and ultrasound markers have been reported, with the aim of estimating the number of gonadotrophin-responsive or ‘selectable follicles’ more accurately. The endocrine markers include factors produced by the developing follicles [oestradiol, inhibin B and anti-Müllerian hormone (AMH)] or hormones under the inhibitory control of these factors [follicule-stimulating hormone (FSH)]. The ultrasound markers are antral follicle count, ovarian volume and ovarian vascularity. The sensitivities, specificities and predictive values of these tests have been evaluated in many studies by correlating the test results with the number of oocytes retrieved, poor or exaggerated ovarian response, and pregnancy or livebirth rates during ART (Broekmans et al 2006).
Serum follicle-stimulating hormone
Early-follicular-phase FSH is the most widely used marker of ovarian reserve, and women with raised FSH levels (>10–15 IU/l) are more likely to have a reduced ovarian response and less successful ART outcome (Scott et al 1989, Sharif et al 1998). A meta-analysis of 21 studies looking at the value of basal FSH in the prediction of IVF outcome concluded that the performance of basal FSH as a screening test is limited in predicting poor ovarian response and non-pregnancy. Predictions with a substantial shift from pre-FSH-test probability to post-FSH-test probability are only achieved at extremely high cut-off levels (Bancsi et al 2003). Moreover, the cycle-to-cycle variability of basal FSH levels limits the reliability of a single measurement for assessment of ovarian reserve. However, it is important to note that ovarian response and pregnancy rates during IVF are low in women with high intercycle variability (Scott et al 1990) or who demonstrate abnormal FSH levels in any menstrual cycle (Abdalla and Thum 2006).
Oestradiol
Measurement of basal oestradiol in addition to FSH is recommended to improve predictive accuracy. Premature elevation of the oestradiol level due to advanced follicular development and early selection of a dominant follicle may tend to suppress the FSH level, thus masking a rise that might otherwise reflect a low ovarian reserve (Frattarelli et al 2000). An elevated level of basal oestradiol (≥60 pg/ml), even in the presence of a normal FSH level, is associated with increased risk of cycle cancellation due to poor ovarian response (Evers et al 1998). However, the use of serum oestradiol estimation for ovarian reserve assessment is limited by the fact that some women with a normal ovarian reserve may have an occasional accelerated cycle with FSH levels of mid-follicular range in their true early-follicular phase (Frattarelli et al 2000). Furthermore, elevated oestrogen may simply reflect the presence of functional ovarian cysts.
Inhibin B
Inhibin B is principally produced by the granulosa cells of the developing cohort of antral follicles during the luteal–follicular transition. Its level in the early-follicular phase is considered to be indicative of the quantity or quality of developing follicles (Hall et al 1999). A low level (<45 pg/ml) of early-follicular-phase inhibin B may predict a poor ovarian response (Seifer et al 1997). However, the reliability of its measurement has been questioned because of significant intercycle variability (McIlveen et al 2007).
Anti-Müllerian hormone
Studies have shown that AMH is a promising serum marker of ovarian reserve (van Rooij et al 2002). AMH, a member of the transforming growth factor-β family of growth and differentiation factors, is primarily produced by the preantral and small antral follicles in women of reproductive age. The serum level of AMH is indicative of the growing follicle pool (de Vet et al 2002). While AMH is highly predictive of potential poor or exaggerated responders to ovarian stimulation during ART, its accuracy to predict the occurrence of pregnancy after one cycle of ART is only marginal (Broekmans et al 2008). Recent studies have suggested that AMH levels vary minimally between menstrual cycles and are cycle independent (Fanchin et al 2005, La Marca et al 2006). Therefore, AMH measurement could be undertaken during any cycle and at any time during the cycle for adequate prediction of ovarian response, and this makes it an attractive marker for routine use. However, there are potential limitations to the regular use of AMH as a marker of ovarian reserve because of different cut-off levels reported in different studies. Currently, there is no international assay standard for AMH measurement, which may contribute to the discordance between different studies and make comparison between laboratories quite difficult. Once the available assays are standardized and automated analysis systems are developed, AMH has the potential to become the test of choice for ovarian reserve.
Antral follicle count
Antral follicle count (AFC) is the most significant predictor of ovarian response among the ultrasound markers (Kwee et al 2007, Jayaprakasan et al 2009), although decreased ovarian volume (<3 cm3) and stromal blood flow are also implicated for poor treatment outcome during ART. The number of gonadotrophin-responsive antral follicles measuring 2–10 mm can be measured using two- or three-dimensional ultrasound with an acceptably high level of agreement both between and within observers (Jayaprakasan et al 2008a). A total follicle count of between seven and 22 is generally considered as the optimum cut-off level for the prediction of poor and exaggerated ovarian response, respectively. AFC measurement can be performed either in the early-follicular phase of the cycle before treatment begins or after downregulation with similar predictive accuracy (Jayaprakasan et al 2008b). However, assessment prior to treatment has an additional advantage in that it provides an opportunity for pretreatment evaluation of the pelvis to screen for pathology. AFC and AMH are currently the best two predictors of ovarian reserve among all the endocrine and ultrasound markers, and are equally predictive of poor ovarian response during ART (Jayaprakasan et al 2010). AFC is currently the test of choice for ovarian reserve assessment as it is easy to perform and due to inherent availability of ultrasound machines.
Ovarian reserve tests including AFC and AMH have limited value in the prediction of non-conception despite their adequate capacity to predict ovarian response during ART (Broekmans et al 2006). Pregnancy may occur even at extreme cut-offs for an abnormal test result; therefore, IVF treatment cannot be denied based on these tests, especially in participants who are seeking their first cycle of treatment (Broekmans et al 2007). However, the identification of participants who are likely to respond poorly during IVF treatment is clinically relevant, as a couple can be counselled accordingly. They can be made aware that they have an increased chance of cycle cancellation and a significantly lower chance of success, allowing an informed decision to be made. Such prediction also allows clinicians to formulate individualized treatment protocols to improve or at least maximize ovarian response.
Evaluation of male partner
In order to give adequate counselling to couples and their families, genetic tests should be performed before, during or after ART in cases such as women with Turner’s syndrome, men with 47XXY, men or women with structural chromosomal aberrations, and men with either Yq11 deletion or congenital bilateral absence of the vas deferens (ESHRE Capri Workshop Group 2000).
Clinical Management of the Treatment Cycle
The main components of typical conventional ART include:
Normal folliculogenesis
This involves several important and inter-related steps.
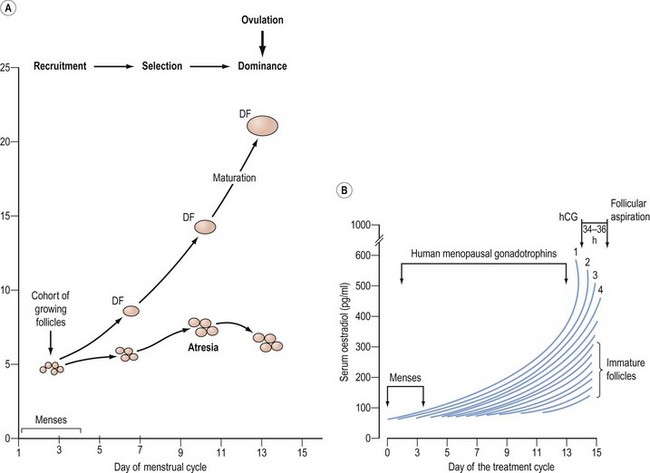
Follicular development beyond the antral stage depends on the concentration of FSH in the circulation. Once a threshold level has been attained, follicular growth beyond 4 mm occurs. The interval during which FSH remains elevated above the threshold level can be regarded as a window through which a follicle must pass to avoid atresia. The width of the window will therefore determine the number of follicles that can be selected for ovulation (Figure 22.2). The preovulatory luteinizing hormone (LH) surge is triggered by the positive feedback of oestradiol from the dominant follicle, as well as other follicular contributory factors. Ovulation occurs 24–36 h after the onset of the LH surge.
Pituitary downregulation
In the conventional ART protocol, it is standard practice to use a continuous and supraphysiological dose of GnRH agonist to obtain control over the hypothalamic–pituitary–ovarian axis. GnRH agonists cause an initial flare response, characterized by increased gonadotrophin secretion, due to upregulation of GnRH receptors. However, prolonged administration of GnRH agonists induces downregulation of GnRH receptors. This prevents a premature surge in LH and subsequent spontaneous ovulation with luteinization, which occurs in up to 23% of cycles when gonadotrophins alone are used and facilitates the timing of oocyte retrieval. The use of GnRH agonists in ART has been shown to increase the number of oocytes retrieved, improve the pregnancy rate and significantly reduce the chance of cycle cancellation (Hughes et al 1992).
Two different GnRH agonist protocols are used in most assisted conception units: long and short protocols. In the long protocol, GnRH agonists (buserelin or nafarelin) are started in the mid-luteal phase (day 21) of the previous menstrual cycle to achieve pituitary downregulation in approximately 8–21 days, after which gonadotrophins are commenced. GnRH agonists are administered for approximately 10–14 days in the short protocol. In both regimens, GnRH agonists are administered daily until the day of hCG or LH injection to trigger oocyte maturation. The short protocol takes advantage of the initial flare effect, which can be utilized to augment the ovarian response to gonadotrophin stimulation. However, a systematic review of 26 randomized-controlled trials found an increased clinical pregnancy rate per cycle and fewer cycle cancellations with the long protocol compared with the short protocol (Daya 2000). Therefore, the long GnRH agonist protocol is generally recommended in most ART cycles.
Use of the long GnRH agonist protocol often prolongs the stimulation phase, resulting in increased requirement for gonadotrophins and increased treatment cost in addition to causing undesirable side-effects of hypo-oestrogenism. It may also be associated with poor response in some patients, as well as introducing a higher risk of ovarian hyperstimulation syndrome (OHSS). Some of the disadvantages can be obviated with the use of GnRH antagonists, such as cetrorelix and ganirelix. GnRH antagonists induce immediate pituitary downregulation by competitively binding to GnRH receptors, and avoid the flare effects or the need for prolonged treatment associated with GnRH agonist protocols. Two different regimes have been described. The multiple-dose protocol involves the administration of 0.25 mg cetrorelix or ganirelix daily from day 6–7 of stimulation, or when the leading follicle is 14–15 mm, until hCG/LH administration. The single-dose protocol involves the single administration of 3 mg cetrorelix on day 7–8 of stimulation. GnRH antagonist protocols are therefore short and simple, but more importantly they reduce the incidence of severe OHSS. However, the clinical pregnancy rates following IVF treatment were significantly lower with GnRH antagonist use compared with the long GnRH agonist protocol [odds ratio (OR) 0.82, 95% confidence interval (CI) 0.68–0.97] (Al-Inany et al 2007), although data from units with experience of the GnRH antagonist protocol are encouraging. More recent trials of GnRH antagonists have reported better pregnancy rates than earlier trials, which used antagonist protocols that would now be recognized as suboptimal.
Controlled ovarian stimulation
Genetic and molecular engineering has led to the production of recombinant human FSH (rFSH) with high purity (>99%), high specific bioactivity (>10,000 IU/mg protein) and absent intrinsic LH activity which is suitable for intramuscular or subcutaneous administration (Mannaerts et al 1991). Two different rFSH preparations are commercially available: follitropin alpha (Gonal F) and follitropin beta (Puregon). These two rFSH preparations differ in that follitropin alpha has a more acidic isoform profile than follitropin beta due to a slight difference in its carbohydrate component. Consequently, they differ in metabolic clearance, half-life and biological activity, but both are equally effective during ART cycles in terms of livebirth rates. A number of well-designed randomized-controlled trials have compared both preparations of rFSH against HMG in their clinical effectiveness during conventional IVF with the long GnRH agonist protocol. While none of them individually showed any statistically significant difference in livebirth rates between the two treatment arms, two recent systematic reviews have demonstrated a significant 4% increase in livebirth rate in the HMG arm (Al-Inany et al 2008, Coomarasamy et al 2008). However, the results of the meta-analysis need to be interpreted with caution because of the clinical heterogeneity of the trials; therefore, a large multicentre randomized double-blind trial is warranted. Moreover, such studies should consider reporting the more clinically relevant cumulative livebirth rates as the primary outcome.
Recombinant DNA technologies have also made it possible to produce LH (rLH). Due to the potential role of LH in follicular development according to the two-cell theory of gonadotrophin system, supplemental rLH has been suggested to improve IVF outcome if rFSH is used for ovarian stimulation. However, a recent systematic review of randomized trials failed to demonstrate any difference in livebirth rates with adding rLH to the rFSH protocol (Kolibianakis et al 2007). Although it is possible that rLH supplementation may be beneficial in a subset of the IVF population, such as poor responders (Mochtar et al 2007), its generalized use is currently limited.
The collective evidence from many studies suggests that 150–225 IU/day gonadotrophin is the appropriate starting dose for most women undergoing conventional IVF treatment. The majority of units use a daily dose according to women’s age and the presence or absence of polycystic ovaries: 150 IU in women under 30 years of age or with polycystic ovaries, 225 IU for those between 30 and 39 years of age, and 300 IU for those aged 40 years or over. The lowest possible dose to achieve the optimum ovarian response should be used to reduce the risks of ovarian hyperstimulation. Although there is no consensus on what constitutes optimum ovarian stimulation, a recent study has reported that the implantation rate is maximum when 10 oocytes are retrieved following conventional IVF using the long downregulation protocol (Verberg et al 2009a).
Recently, mild ovarian stimulation protocols have gained a lot of interest in the field of ART, with the current trend of limiting the number of embryos transferred reducing the need for large numbers of oocytes. The principal aim with this approach is to reduce the number of developing follicles and thereby minimize the adverse effects of ovarian stimulation, particularly OHSS and multiple pregnancies. Three reported mild stimulation protocols include clomiphene citrate alone or in combination with gonadotrophins, delayed commencement (day 5 of the cycle) of gonadotrophins with GnRH antagonist co-medication, and late follicular replacement of FSH with administration of hCG/LH (Verberg et al 2009b). All of these protocols have been shown to reduce the gonadotrophin dosage and have the potential to reduce the cost of treatment and patient distress associated with conventional ART. As expected, the ongoing pregnancy rates/livebirth rates per cycle have been lower compared with the conventional protocol, but similar effectiveness could be achieved with more treatment cycles.
Oocyte Retrieval
It is important to provide effective anaesthesia and analgesia for transvaginal oocyte recovery, as this is painful. No techniques for anaesthesia, analgesia or sedation are free from side-effects. Whichever technique is used, recognized standards of practice should be adhered to and all IVF professionals should follow the safe practice of administering sedative drugs published by the Academy of Medical Royal Colleges (2001). Conscious sedation should be offered to all women having the procedure as it is a safe and acceptable method of providing analgesia.
Technique
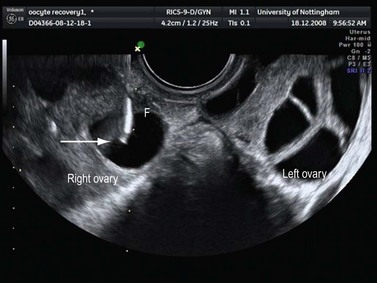
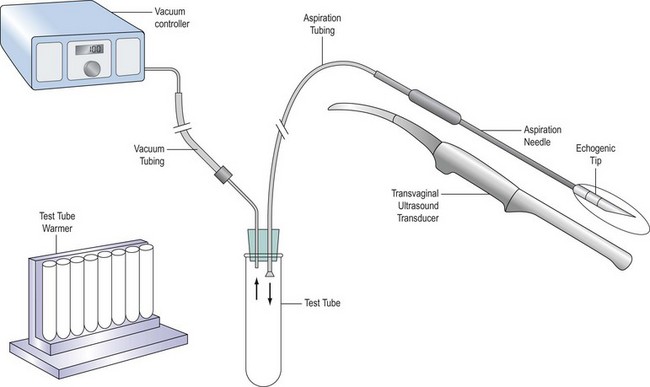
Several types of aspiration needle are available. They may have a single or double lumen to enable aspiration and flushing through different routes. The needle is usually 16-guage and must have a very sharp tip to enable easy puncture of mobile ovaries; the distal 2 cm should be roughened to enhance ultrasound visualization (Figure 22.3). The needle is connected to a test tube by tubing, and suction is applied either from a foot-operated pump (Figure 22.4) or manually. The ultrasound transducer (Figure 22.5) is enclosed in a special sterile condom and plastic sleeve prior to insertion into the vagina, and should be cleaned thoroughly with a damp cloth after each procedure.
Generally, very few technical difficulties are encountered during vaginal egg collection. The main risks of transvaginal oocyte recovery are pelvic infection (0.6%) and bleeding (>100 ml in 0.8% cases) (Bennett et al 1993), which may be serious, sometimes even fatal. Appropriate preoperative vaginal preparation and minimizing the number of repeated vaginal penetrations may serve to lower the risk of infection. While there is no evidence that routine antibiotics reduce the risk of infection, the administration of an intravenous bolus of antibiotic is generally recommended for women with a history of severe pelvic inflammatory disease or if an endometrioma is punctured. Intestinal, vascular, uterine and tubal injuries with the aspiration needle have also been reported. Bleeding and infections may be serious, sometimes even fatal, complications.
Laboratory Techniques
In cases of ICSI, meiotic maturity is assessed after denudation; only the mature oocytes are injected with sperm, following immobilization. Fertilization, as determined by the presence of two pronuclei, is assessed 18–20 h after insemination. On day 2 or 3, based on the cleavage rate, the size, shape, symmetry and cytoplasmic appearance of the blastomeres and the presence or absence of nucleus, embryo quality is graded by embryologists as grade 1, 2, 3 or 4 (Van Royen et al 1999). Grade 1 and 2 embryos are considered to be of high quality. While ET is performed with one or two of the best-available embryo/s, regardless of their grading, only top-quality (grade 1 and 2) embryos are considered eligible for freezing and this option is then offered to the couple.
Embryo Transfer
ET is a critical step in determining the final outcome of the treatment. The convention has been to replace embryos on the second or third day post insemination, when the embryos are usually at the two- to eight-cell stage of cleavage. With improvements in culture media, there is an increasing tendency for delaying ET with the aim of improving implantation rates. While there is no improvement in livebirth rates (OR 1.07, 95% CI 0.84–1.37) with delaying ET from day 2 to day 3 (Oatway et al 2004), transfer of embryos at the blastocyst stage (day 5/6) has shown a significant increase in the livebirth rate (OR 1.35, 95% CI 1.05–1.74) compared with transfers on day 2 or 3 (Blake et al 2007). It is a more physiological approach, allowing synchronization of the embryo with the endometrium, and selection of the viable embryos for transfer will be more efficient. However, the rates of embryo freezing are lower and the treatment cancellation rates are higher with blastocyst transfer. However, in certain couples, blastocyst transfer has the potential to favour single ET without compromising the overall success rates, but can significantly reduce the occurrence of multiple pregnancies. The most favoured couples for blastocyst transfer are those with high numbers of eight-cell embryos on day 3, in whom cycle cancellation is not increased.
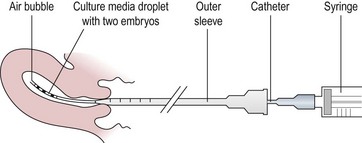
Transcervical embryo replacement into the uterine cavity is a relatively simple procedure, which must be carried out meticulously to ensure appropriate placement of the embryos (Figure 22.6). Variations among clinicians in the technique of ET may influence the pregnancy rate. Avoidance of blood, mucus, bacterial contamination, excessive uterine contractions and trauma to the endometrium is associated with optimal pregnancy and implantation rates after transcervical ET. Transabdominal ultrasonographic guidance to determine the precise depth of embryo placement within the uterus appears to facilitate successful ET and is preferred (Brown et al 2007), although a recent large randomized trial from a single centre did not show any benefit over ‘clinical touch’ transfer (Drakeley et al 2008). The tip of the catheter is placed approximately 1 cm from the uterine fundus so that the embryo/s are expelled gently into the mid-cavity of the uterus. Soft catheters are preferable to rigid catheters as they are less likely to traumatize the cervix or endometrium, or to invoke any uterine contractions. The commonly used soft catheters (Wallace catheters) (Figure 22.7) have a softer inner cannula and a stiffer outer sheath. Occasionally, resistance to pass the soft inner cannula into the uterus, usually at the level of internal os, is encountered; in these cases, the stiffer outer sheath is advanced into the cervical canal to negotiate the resistance, and the inner cannula can be advanced into the uterine cavity. A firmer malleable catheter with a stylet and an outer sheath is another option in difficult cases, where the catheter is advanced up to the level of the internal os. The inner stylet is then removed and the softer cannula loaded with embryos is fed through the outer sheath to advance into the uterine cavity for transfer. The outer sheath or the malleable catheter should never be advanced beyond the internal os.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree