CHAPTER 25 asymmetric intrauterine growth restriction objective means for assessing fetal well-being. systolic pressure ≥140 mm Hg or a diastolic pressure ≥90 mm Hg. amniotic fluid below the normal range for gestational age. amniotic fluid above the normal range for gestational age. gestation greater than 42 weeks. symmetric intrauterine growth restriction fetal growth abnormality resulting in a proportionally small fetus. fatty material found on the fetal skin and amniotic fluid late in pregnancy. • Abdominal circumference (AC). • Head circumference-to-abdominal circumference ratio (HC/AC). • During the early third trimester, the head circumference is slightly larger than the circumference of the abdomen. • During the late third trimester, with the increase of fetal body fat, the abdominal circumference is typically equal to or slightly larger than the head circumference. • Interval fetal growth can be determined with ultrasound examinations a minimum of 3 weeks apart. • In the last 3 months of pregnancy, the fetus will grow an additional 4 inches in length and gain an additional 2000-2800 g in weight at 100-200 g per week. • Distal femoral epiphysis (DFE) is visualized around 32 gestational weeks. • Proximal tibial epiphysis (PTE) is visualized around 35 gestational weeks. • Results from insufficient fetal nutrition. • Defined as a fetal weight at or below the 10th percentile for gestational age. • No single reliable criterion is available to diagnose intrauterine growth restriction. • Associated with maternal hypertension. • Evaluation of the amniotic fluid volume, estimated fetal weight, and maternal blood pressure results in the most accurate diagnosis. • The liver is one of the most severely affected fetal organs. • Decrease in liver size results in a decrease in abdominal circumference. Intrauterine Growth Restriction • Fetal weight above 4000 g or above the 90th percentile for gestational age. • Fetuses of diabetic mothers are likely to display organomegaly, whereas fetuses of nondiabetic mothers will demonstrate normal growth. • Fetuses of diabetic mothers demonstrate a higher mortality rate. • Normal volume of amniotic fluid varies with gestational age. • Early in gestation, the major source of amniotic fluid is the amniotic membrane. • As the embryo and placenta develop, fluid is produced by the placenta and fetus. • After 16 gestational weeks, the fetus is the major producer of amniotic fluid. • Normal volume of amniotic fluid increases progressively until about 33 gestational weeks. • During the late second and early third trimester, the amniotic fluid volume appears to surround the fetus. • By the late third trimester, the amniotic fluid displays as isolated fluid pockets. • Regulated by the production of fluid, swallowing of fluid (removal), and fluid exchange within the lungs, membranes, and cord. • Normal lung development depends on the exchange of amniotic fluid within the lungs. • Oligohydramnios increases risk of fetal death and neonatal morbidity. • Transducer must remain perpendicular to the maternal coronal plane and parallel to the maternal sagittal plane. • Fluid pocket must be free of umbilical cord or any fetal part. Methods of Assessing Amniotic Fluid Volume Abnormal Amniotic Fluid Volume
Assessment of the third trimester
Third-trimester measurements
Fetal growth
Decrease in fetal growth
Intrauterine growth restriction
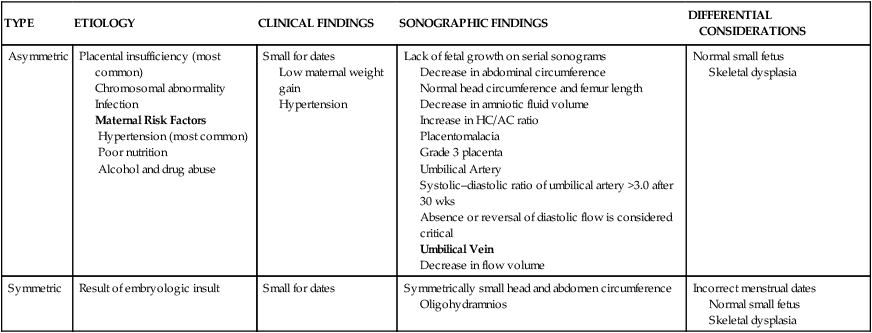
TYPE
ETIOLOGY
CLINICAL FINDINGS
SONOGRAPHIC FINDINGS
DIFFERENTIAL CONSIDERATIONS
Asymmetric
Placental insufficiency (most common)
Chromosomal abnormality
Infection
Maternal Risk Factors
Hypertension (most common)
Poor nutrition
Alcohol and drug abuse
Small for dates
Low maternal weight gain
Hypertension
Lack of fetal growth on serial sonograms
Decrease in abdominal circumference
Normal head circumference and femur length
Decrease in amniotic fluid volume
Increase in HC/AC ratio
Placentomalacia
Grade 3 placenta
Umbilical Artery
Systolic–diastolic ratio of umbilical artery >3.0 after 30 wks
Absence or reversal of diastolic flow is considered critical
Umbilical Vein
Decrease in flow volume
Normal small fetus
Skeletal dysplasia
Symmetric
Result of embryologic insult
Small for dates
Symmetrically small head and abdomen circumference
Oligohydramnios
Incorrect menstrual dates
Normal small fetus
Skeletal dysplasia
Increase in fetal growth
Macrosomia
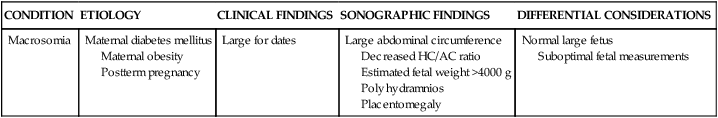
CONDITION
ETIOLOGY
CLINICAL FINDINGS
SONOGRAPHIC FINDINGS
DIFFERENTIAL CONSIDERATIONS
Macrosomia
Maternal diabetes mellitus
Maternal obesity
Postterm pregnancy
Large for dates
Large abdominal circumference
Decreased HC/AC ratio
Estimated fetal weight >4000 g
Polyhydramnios
Placentomegaly
Normal large fetus
Suboptimal fetal measurements
Amniotic fluid
Amniotic fluid volume
Measuring amniotic fluid volume
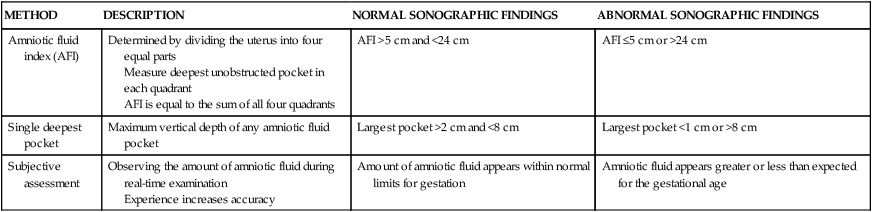
METHOD
DESCRIPTION
NORMAL SONOGRAPHIC FINDINGS
ABNORMAL SONOGRAPHIC FINDINGS
Amniotic fluid index (AFI)
Determined by dividing the uterus into four equal parts
Measure deepest unobstructed pocket in each quadrant
AFI is equal to the sum of all four quadrants
AFI >5 cm and <24 cm
AFI ≤5 cm or >24 cm
Single deepest pocket
Maximum vertical depth of any amniotic fluid pocket
Largest pocket >2 cm and <8 cm
Largest pocket <1 cm or >8 cm
Subjective assessment
Observing the amount of amniotic fluid during real-time examination
Experience increases accuracy
Amount of amniotic fluid appears within normal limits for gestation
Amniotic fluid appears greater or less than expected for the gestational age
ABNORMALITY
ETIOLOGY
SONOGRAPHIC FINDINGS
DIFFERENTIAL CONSIDERATIONS
Oligohydramnios
Fetal
Genitourinary tract abnormality
Intrauterine growth restriction
Maternal
Poor nutrition
Placenta insufficiency
Premature rupture of membranes
AFI below 5 cm
Below the 5th percentile for gestational age
Largest single pocket below 1 cm
Poor fetal–fluid interface
Volume <300-500 mL
Lower limits of normal
Premature rupture of membranes
Polyhydramnios
Fetal Anomalies
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access
