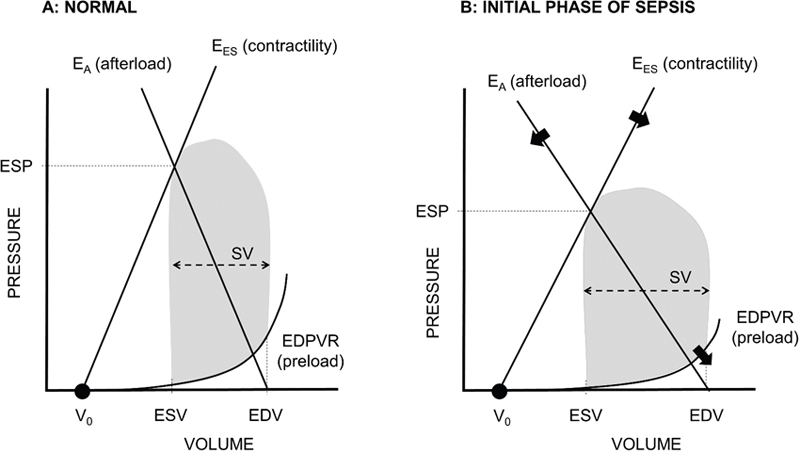
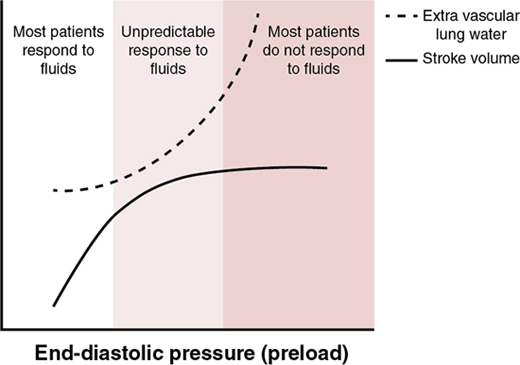
Koert de Waal, Istvan Seri Key points Sepsis remains a leading cause of morbidity and mortality in the neonatal population. There is a strong inverse relationship between the incidence of sepsis, gestational age, and birth weight. The incidence and mortality in term or late preterm infants with sepsis has slowly decreased over time, but the incidence and case-fatality rate remain high in very-low-birth-weight (VLBW) infants.1–5 This chapter addresses the clinical and hemodynamic presentation and cardiovascular and antibiotic management of neonates, with sepsis caused by bacterial infection. Primarily because of scant hemodynamic data, the clinical and cardiovascular presentation of neonates with sepsis caused by viral (herpes virus, enteroviruses, etc.) or fungal infection might be somewhat different. Currently, there is no unified consensus definition of neonatal sepsis.6,7 Definitions of neonatal sepsis in the literature emphasize microbiological evidence of infection, without consideration for potential organ dysfunction, and include general clinical practice items such as treatment duration with antibiotics. The last pediatric consensus definition was presented in 2005 and incorporated the presence of evidence for a systemic inflammatory response.8 However, this definition is not applicable to the newborn population as many neonates with septic shock would not qualify, similar to what was found in adults.9,10 The “Sepsis-3 Group” has recently defined sepsis in adults as a life-threatening organ dysfunction caused by a dysregulated host response to infection, and septic shock is defined as a subset of sepsis in which underlying circulatory and cellular/metabolic abnormalities are profound enough to significantly increase mortality.10 It would not be unreasonable to use a similar but adapted version for septic shock in newborns, but some questions still remain. First, the host response of newborns is different from that of adults. The fetus lives in a unique environment where protection against infection is paramount. Yet, the fetus also must avoid the development of harmful, dysregulated inflammatory immune responses that could lead to preterm birth. Birth is the transition from the intra-uterine environment with low-grade presence of maternal bacteria essential for the development of, among others, the immune system to a new environment abundant in foreign antigens and pathogens requiring a balanced immunological response. Much remains to be understood about the newborn’s immune response to infection, and whether these biochemical processes can be used in the early detection of a dysregulated immune response and/or to guide treatment of neonatal infections.11,12 Second, there is no consensus on the definition of a life-threatening organ dysfunction in newborns. Newborn illness score systems with a focus on acute physiology like the SNAPPE or CRIB scores have generally placed much emphasis on risk assessment on the first postnatal day and have not been validated for use thereafter.13 Sepsis-specific scores like the NEOMOD have been tested and modified for performance but are infrequently used and reported in the literature.14 Pediatric organ dysfunction scores have shown increased mortality for the same scoring range in newborns and older infants, but newborns showed different primary organ involvement with acute illness.15 The neonatal sequential organ failure assessment score (nSOFA) uses parameters of respiratory support, oxygenation, cardiovascular support, and platelet count.16 When applied to preterm infants with late-onset sepsis, the maximum nSOFA score at 6 hours after the clinical diagnosis was established showed a strong association with mortality and thus could be proposed as an operational definition of organ dysfunction in this population.17 Although the nSOFA score has an excellent diagnostic accuracy for mortality due to sepsis and all-cause mortality, its validity is highly dependent on local guidelines for the use of systemic steroids and criteria for intubation. A subsequent study revealed a wide variance between centers in all-cause mortality of preterm infants with high nSOFA scores, questioning its generalizability.18 Finally, the ability of translating the “Sepsis-3” definition and its tools to the newborn population also depends on data regarding sepsis mortality. However, wide ranges of mortality have been reported for sepsis in newborns. Recent epidemiological data from research networks showed that mortality from early-onset sepsis (EOS) and late-onset sepsis (LOS) in very-low-birth-weight (VLBW) infants was in the range of 12–33% and 4–16%, respectively.3,5,19,20 Risk factors for developing EOS and LOS in VLBW infants have been amply described, but limited data are available on risk factors for death due to sepsis. Decreasing gestational age, birth weight, and the presence of gram-negative organisms are associated with higher risk of mortality due to sepsis, but more data are required to better understand the risk factors involved in the progression from sepsis to septic shock.21,22 The “Sepsis-3” definition defines septic shock as a circulatory and cellular/metabolic abnormality profound enough to increase mortality. In the neonatal literature and for logistical reasons septic shock is often defined as sepsis with hypotension requiring catecholamines. The rate of infants who progress from sepsis to septic shock is reported as 26% for EOS and between 9 and 22% for LOS and depends on the infective agent.3,23,24 Most studies did not report case fatality separately for infants with septic shock. Gorantiwar et al. presented a decade’s worth of data from a single center in Australia and reported a mortality rate of 40% in preterm infants with LOS and sepsis shock, suggesting that mortality is significantly higher when shock develops. In a yet unpublished retrospective study of similar design our group found a 33% mortality rate for preterm infants with EOS. However, the rate increased to 67% in infants who progressed from sepsis to septic shock.25 Data on other aspects commonly associated with mortality, such as lactate levels and lactate clearance, fluid load, fluid accumulation, and multi-organ dysfunction, have been sparsely reported for the neonatal population with sepsis.26,27 Phenotyping of neonatal sepsis might be possible with accurate documentation of timing of treatments, biochemical profiles, or reporting of progression from sepsis to septic shock.28,29 In summary, there is a need to develop a better understanding of the clinical, phenotypic, and even genotypic factors associated with progression from sepsis to septic shock in neonates with EOS or LOS, before we can appropriately define mortality and/or describe the appropriateness and efficacy of treatment modalities and short- and long-term outcome in the affected patient population. Sepsis starts with a disruption of the finely tuned immunological balance of inflammation and anti-inflammation, driving the vascular response to sepsis and leading to ineffective tissue oxygen delivery and extraction due to inappropriate vasodilatation with preserved or increased cardiac output. This hemodynamic effect, along with the infectious agent– and/or its toxin-induced direct cellular metabolic derangement, is also responsible for the loss of the cellular oxygen demand-delivery coupling. The increased capillary leak and generalized vasodilation result in an absolute and relative decrease in effective circulating blood volume, respectively, resulting in load-driven alterations in left and right ventricular function. The decrease in effective circulating blood volume leads to a decrease in circulatory filling pressure (reduced preload), while the inappropriate vasodilatation with low systemic vascular resistance leads to reduced afterload and lower organ perfusion pressure.30 Although the cascade of inflammatory activation often leads to cardiomyocyte dysfunction with reduced myocardial contractility, the initial phase of sepsis is often described as a patient with high systemic blood flow, i.e., warm shock.31 The pressure-volume curve of the heart is operating at lower pressures but with larger stroke volume due to the vascular changes affecting the preload and afterload (Figure 21.1). The interaction between the left ventricle and the arterial system, known as ventriculo-arterial coupling (VAC), is one of the main determinants of cardiovascular function during sepsis and can be used as a marker to target treatment in adults.32,33 Other hemodynamic changes during sepsis in adults include diastolic dysfunction, combined left and right ventricular dysfunction, and pulmonary hypertension. Of note, pulmonary hypertension and, in particular, diastolic dysfunction are significantly associated with increased mortality and warrant thorough investigation in the newborn population as well.34–37 In summary, vasodilatation and the associated relative hypovolemia and altered ventriculo-arterial interactions are key hemodynamic factors in adults with sepsis, especially in the early phases. Stroke volume is initially high, and cardiac dysfunction (systolic and/or diastolic) and pulmonary hypertension are common. Although early studies in newborns showed that septic shock presented with reduced cardiac output and increased systemic and pulmonary vascular resistance (i.e., “cold shock” with PPHN), the generalizability of this concept has been challenged by the findings of recent studies. Acknowledging the maturational differences of the structure of all three layers of the vascular wall and the myocardium, newborns, and especially preterm infants, are often in a pro-inflammatory state following delivery. Accordingly, one might expect to see the same hemodynamic pathophysiology in sepsis as found in adults. Kharrat et al. recently summarized papers describing hemodynamics in the neonatal population with sepsis.38 The definition of sepsis varied per studies and some even included infants without a positive blood culture. In addition, most studies were performed in countries with a relatively high perinatal sepsis rate and the oldest study reviewed was published only 12 years ago. An additional confounding variable to be considered when interpreting the findings was the fact that the timing of the ultrasound assessment after the onset of sepsis was not always reported. A summary of the 14 studies included is presented in Table 21.1.25,39–50 Systemic blood flow was predominantly high, assessed through either ventricular output (the Vti method) or volumetric changes (ejection fraction, stroke volume). Most studies commented on the presence of cardiac dysfunction (systolic, diastolic, and/or global cardiac function) and some reported the presence of pulmonary hypertension. Overall, the findings support the assumption that newborns with sepsis mostly present with a hemodynamic pattern characteristic of warm shock and added cardiac dysfunction and pulmonary hypertension, similar to that found in adults. Only two studies presented longitudinal hemodynamic data in their cohorts. de Waal et al. described a cohort of 20 preterm infants (median gestational age of 27 weeks) with LOS and at least two clinical signs of cardiovascular compromise. The infants underwent echocardiography within 2 hours of presentation, which was then repeated every 12 hours until clinical recovery or death.39 All infants presented with high systemic blood flow, suggesting warm shock as the main hemodynamic presentation. Of note is that early and remarkable hemodynamic changes took place in the infants who died; specifically, their hemodynamic presentation changed from warm shock to cold shock, with a sudden decline in cardiac output and increase in systemic vascular resistance. This change occurred in most cases within 12 hours of the onset of sepsis, also highlighting the importance of serial echocardiographic assessments of infants with septic shock. Only systemic blood flow was assessed in this study, so no data could be presented on cardiac dysfunction or pulmonary hypertension. Saini et al. investigated 52 preterm infants (median gestational age of 31 weeks) with fluid-resistant septic shock around postnatal day 4.42 Half of the patients presented with a positive blood culture, while the others had clinically diagnosed sepsis. Nine infants (17%) sustained blood pressure in the normal range, while the others (83%) progressed to septic shock. Both left and right ventricular output were elevated at baseline, and the patients had a shortened isovolumetric relaxation time suggesting diastolic dysfunction. Repeat measurements 30–40 minutes after start of dopamine or dobutamine showed surprisingly little changes in hemodynamics. This may relate either to the repeat measures being taken too early, lack of appropriate titration of the drugs, incorrect physiologic choice (vasopressor preferred circulation, e.g., epinephrine, norepinephrine, or vasopressin), or – although less likely – shock had already progressed to the point of no return in this cohort, with a very high (81%) mortality rate. In summary, more data and trials with a more sophisticated design are needed. In the ideal study all infants with suspected sepsis would be followed using a comprehensive hemodynamic monitoring system and interrogated with echocardiography and vascular ultrasound every 6 hours until resolution of the clinical signs that triggered the sepsis evaluation. In addition, careful volume resuscitation and testing for the use of the most appropriate vasopressor-inotrope are needed.51 Data collection should include clinical and hemodynamic response to each treatment in culture-positive patients. This huge undertaking is unlikely to occur as it is likely impossible to be performed as a single-center study. An alternative approach would be development of an international multicenter patient registry until a well-designed and executed multicenter study is performed. The basic steps in the management of neonates with bacterial sepsis include clinical recognition, microbiological evaluation, starting appropriately chosen antibiotics tailored according to the sensitivity of the identified bacterium, and appropriate cardiorespiratory support if the condition progresses to septic shock. Sepsis can present with a wide range of clinical signs and symptoms.7 Increased respiratory support, apnea, lethargy, the presence of a central line, and capillary refill time >2 seconds were common in preterm infants with LOS.52 Yet these clinical signs and presentations were not universally seen. Due to the non-specific nature of clinical signs and symptoms at the start of sepsis, it can take the clinical team 5–12 hours to recognize the need for antibiotics.24 Various biomarkers are available to help the clinician (C-reactive protein, procalcitonin, cell surface antigens, cytokines), but their diagnostic advantage in preterm infants with LOS remains controversial.53,54 The utilization of heart rate characteristic monitoring tools has shown promise in earlier detection and initiation of antibiotic treatment, resulting in decreased sepsis-associated mortality in preterm neonates.53 Blood pressure, and especially changes in blood pressure, can be used to signify the start of the uncompensated phase of septic shock. Zhu et al. described blood pressure changes in a cohort of 147 preterm infants with culture-positive (excluding coagulase-negative staphylococcus) LOS. They found a decrease (up to 47%) in mean blood pressure in the infants who died and minimal blood pressure changes in the infants who survived. Changes were seen in both systolic (−24%) and diastolic (−21%) blood pressure in the first 12 hours after sepsis work-up was completed. Importantly, baseline mean blood pressure value in mmHg before the infants became sick, as well as shortly thereafter, was well above the number of corrected gestational age in weeks. Thus the fairly controversial rule-of-thumb of utilizing the mean blood pressure value in mmHg less than gestational age in weeks to initiate treatment should not be used in neonates with LOS, but rather use the change in blood pressure. Bedside cardiac ultrasound is the most commonly used hemodynamic monitoring tool in sepsis in adults, children, and newborns, as it can provide information on systemic blood flow (high or low), myocardial function, and the presence of intracardiac and extracardiac shunts and acute pulmonary hypertension. Furthermore, with longitudinal scans, the clinical team can diagnose hemodynamic changes from warm shock to cold shock at an early stage and modify the treatment from vasopressor-inotrope to inotrope/lusitrope treatment where needed.55 Training, guidelines, and accreditation of bedside clinicians using this monitoring technique are available, as the value of bedside neonatal cardiac ultrasound has been increasingly recognized in the last decade.56 As described earlier, the hemodynamic abnormalities in septic shock are inappropriate and dysregulated vasodilation, a relative and, later in the course, also an absolute decrease in circulating blood volume and increased systemic blood flow with impaired myocardial contractility. Fluid therapy is used as a first step to counteract this pathophysiology. However, the efficacy of fluid resuscitation in septic shock has been called into question.57 We have shown that a single fluid bolus in infants with septic shock had variable responses, as was found in other studies.24,42,48 This can be explained by the fact that at high pre-existing preload, a fluid bolus will not increase stroke volume but might cause harm due to accumulation of fluid in the lungs. (Figure 21.2)
Chapter 21: Assessment and management of septic shock and hypovolemia
Introduction
Hemodynamics in sepsis
Hemodynamic response to sepsis in adults
Hemodynamic response to sepsis in newborns
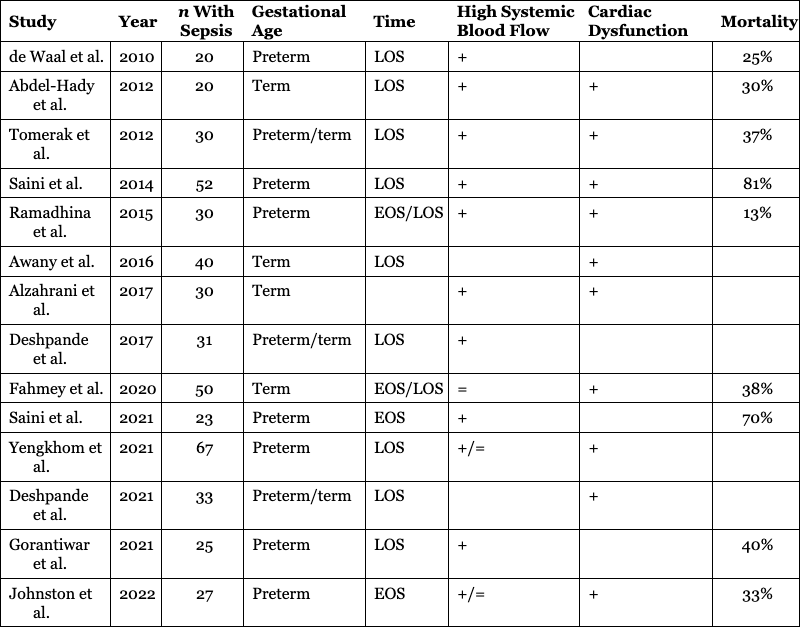
Study
Year
n With Sepsis
Gestational Age
Time
High Systemic Blood Flow
Cardiac Dysfunction
Mortality
de Waal et al.
2010
20
Preterm
LOS
+
25%
Abdel-Hady et al.
2012
20
Term
LOS
+
+
30%
Tomerak et al.
2012
30
Preterm/term
LOS
+
+
37%
Saini et al.
2014
52
Preterm
LOS
+
+
81%
Ramadhina et al.
2015
30
Preterm
EOS/LOS
+
+
13%
Awany et al.
2016
40
Term
LOS
+
Alzahrani et al.
2017
30
Term
+
+
Deshpande et al.
2017
31
Preterm/term
LOS
+
Fahmey et al.
2020
50
Term
EOS/LOS
=
+
38%
Saini et al.
2021
23
Preterm
EOS
+
70%
Yengkhom et al.
2021
67
Preterm
LOS
+/=
+
Deshpande et al.
2021
33
Preterm/term
LOS
+
Gorantiwar et al.
2021
25
Preterm
LOS
+
40%
Johnston et al.
2022
27
Preterm
EOS
+/=
+
33%
Management of neonates with bacterial sepsis
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Assessment and management of septic shock and hypovolemia
Selected Hemodynamic Data in Preterm and Term Infants with Sepsis. Systemic Blood Flow Represents the Interaction Between the Ventricle and the Arterial System and was Assessed with the VTI Method (Right or Left Ventricular Output, Superior Vena Cava Flow) and/or M Mode or Method of Disks (Stroke Volume, Ejection Fraction). Cardiac Dysfunction was Assessed with Tissue Doppler Velocities, Myocardial Performance Index, E:A Ratio, E:e´ Ratio, and/or Tricuspid Annular Plane Systolic or Tricuspid Regurgitation Jet Velocity. Los, Late-Onset Sepsis; EOS, Early-onset Sepsis. For Further Details Regarding Assessment of Cardiovascular Dysfunction Utilizing Ultrasound, See Chapter 10
