Fig. 4.1
Ultrasound and saline infusion revealing filling defects in a patient with AS
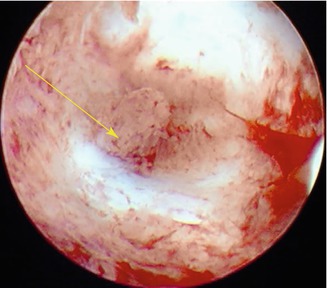
Fig. 4.2
Dense adhesion in the inner cervical area
4.5 Classification
Since the description of AS was made in 1948, several attempts have been made to classify the extent of adhesions and lesions in patients with AS.
To date, several classification schemes are available for classification of the extent of Asherman disease. One of the most widely used is developed on behalf of the American Fertility Society and provides a classification of AS based on extent of the disease, menstrual pattern, and the morphological feature of the adhesions. Both hysteroscopy and HSG could be used for this kind of scoring system (Table 4.1).
Table 4.1
The American Fertility Society classification system for intrauterine adhesions
Classification | Score | |
|---|---|---|
Extent of cavity involved | <1/3 | 1 |
1/3–2/3 | 2 | |
>2/3 | 4 | |
Type of adhesion | Filmy | 1 |
Filmy and dense | 2 | |
Dense | 4 | |
Menstrual pattern | Normal | 0 |
Hypomenorrhea | 2 | |
Amenorrhea | 4 | |
Prognostic classification | Stage 1 (Mild): 1–4 | |
Stage 2 (Moderate): 5–8 | ||
Stage 3 (Severe): 9–12 | ||
More recently, a classification scheme published in 2000 by Nasr et al. illustrated an innovative way to classify AS (Table 4.2). This scoring system includes not only the menstrual symptoms but also the obstetric history of the woman (Nasr et al. 2000). According to this group, clinical history plays a more important role than the extent of the adhesions. The classification scheme provides good correlation in women with mild or severe disease, but not in those with moderate adhesions.
Table 4.2
Clinico-hysteroscopic classification system for intrauterine adhesions
Hysteroscopic findings | Score | |
|---|---|---|
Isthmic fibrosis | 2 | |
Filmy adhesions | >50 % of the cavity | 1 |
<50 % of the cavity | 2 | |
Dense adhesions | Single band | 2 |
Multiple bands | 4 | |
Tubal ostium | Both visualized | 0 |
One visualized | 2 | |
None visualized | 4 | |
Tubular cavity | Sound less than 6 | 10 |
Menstrual pattern | ||
Normal | 0 | |
Hypomenorrhea | 4 | |
Amenorrhea | 8 | |
Reproductive performance | ||
Good obstetric history | 0 | |
Recurrent pregnancy loss | 2 | |
Infertility | 4 | |
Stages | Mild | 0–4 |
Moderate | 5–10 | |
Severe | 11–22 | |
4.6 Management
Treatment of AS should only be considered when there are signs or symptoms of pain, menstrual abnormalities, infertility, or recurrent pregnancy loss. The primary goal of intervention is to restore the volume and shape of the uterine cavity; to facilitate communication between fallopian tubes, uterine cavity, and cervical canal; and to restore reproductive function.
The management strategy of AS is based on four steps:
1.
Surgical procedures
2.
Prevention of the formation of re-adhesions
3.
Restoring a normal endometrium
4.




Postoperative assessment
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


