Chapter 20 Arthritis and Arthralgia
Suspected Rheumatologic Disease
ETIOLOGY
What Causes Joint Pain and Swelling?
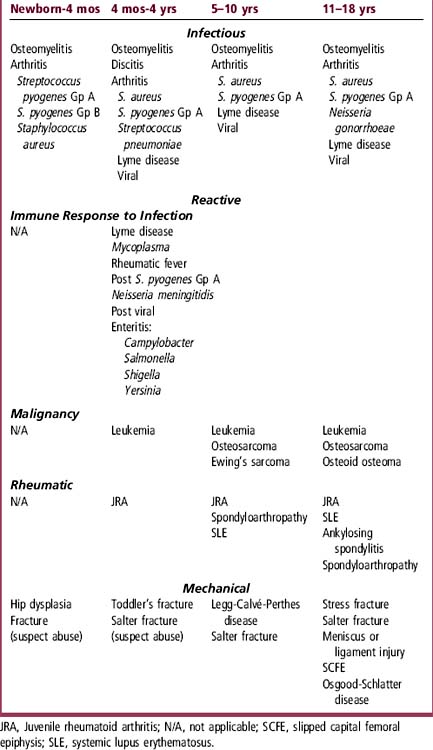
The causes of arthritis and arthralgia in children can be grouped into three major categories: infectious, reactive, or mechanical. The differential diagnosis is based on age (Table 20-1). These clinical presentations should be distinguished from benign, self-limited “growing pains” that typically occur at night in children ages 3 to 6 years and are easily relieved by massage, nonsteroidal antiinflammatory drugs (NSAIDs), or acetaminophen.
How Do Infectious and Reactive Arthritis Differ?
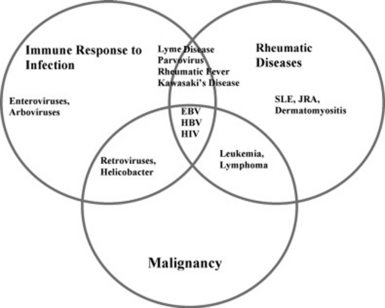
Infectious arthritis results from direct infection of a bone or joint. Reactive arthritis often results from the immune response to infection, as in rheumatic fever. It can also reflect an autoimmune disorder, such as juvenile rheumatoid arthritis, or a malignancy, such as leukemia (Figure 20-1).
What Causes Rheumatologic Disease?
Rheumatologic diseases are autoimmune disorders in patients with the genetic predisposition to develop an exaggerated immune response to drugs, bacteria, viruses, and also to their own cells and tissues. The inciting factor is unknown for most disorders, such as systemic lupus erythematosus (SLE). The most common rheumatologic diseases in children are juvenile rheumatoid arthritis (JRA), SLE, dermatomyositis, and vasculitis (Chapter 70).
What Mechanical Problems Cause Joint Pain?
Knee and hip pain often result from mechanical or traumatic causes (see Chapter 68). Patellar-femoral syndrome and cartilage or ligament injury cause knee pain in active adolescent girls. Osgood-Schlatter disease is a common finding in physically active adolescents. Slipped capital femoral epiphysis (SCFE) occurs in obese adolescent boys, who present with a painful “waddling gait.” Legg-Calvé-Perthes disease is seen in younger boys.
EVALUATION
What Helps Differentiate the Causes of Joint Pain?
Fever: Infection must be considered if fever is present because rapid diagnosis and antibiotic treatment are necessary to prevent joint destruction and sepsis. Patients with reactive arthritis may have fever, but it is uncommon in mechanical disorders. Malignancy also causes fever, arthritis, and bone or joint pain.
Pain location, quality, onset, and duration: Knee pain may be at the site of trauma or may be referred from the hip, so a careful hip examination is warranted. Patients with septic arthritis usually present with toxicity and severe pain within 24 to 48 hours of onset, whereas those with reactive arthritis or mechanical causes often have stiffness and swelling that evolves over days or weeks. Severe diffuse bone pain that is present during the day but worse at night suggests malignancy because expansion of the marrow by leukemic infiltration can cause bone pain weeks or months before blasts are seen on the peripheral smear.
History of prior infections: Many viruses and bacteria activate T cells that cross-react with joint antigens, causing a postinfectious or reactive arthritis (Table 20-1).
Underlying disease: Children with sickle cell anemia may have bone pain with a vasoocclusive crisis.
How Does Septic Arthritis Differ from Reactive Arthritis?
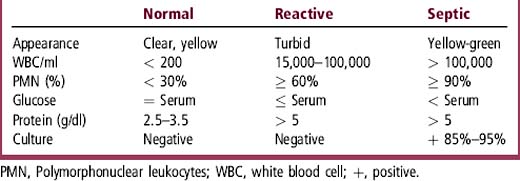
Children with reactive arthritis typically have low-grade fever but are not toxic-appearing. Streptococcus, Mycoplasma, parvovirus, and rubella can cause either direct joint infection or a reactive inflammatory response leading to arthritis. The arthritis of rheumatic fever usually involves the large joints, especially the knee; is painful out of proportion to clinical findings; and often is migratory. It responds dramatically to NSAIDs. Evaluation to exclude cardiac involvement is needed. A “toxic-appearing” febrile child with a swollen, red joint should be presumed to have a septic arthritis (see Chapter 64). Consider arthrocentesis if a limping child has a fever, especially if a septic hip is suspected. Table 20-2 lists synovial fluid findings that distinguish infectious from reactive arthritis.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree