A patient in a minimally conscious state has severely altered consciousness but has definite behavioral evidence of self or environmental awareness. A patient in this state may follow simple commands, make nonreflexive gestures or yes-no responses (regardless of response accuracy), or exhibit purposeful behaviors that are contingent on environmental stimuli. Examples include smiling or crying in response to appropriate stimuli but not neutral stimuli, vocalization or gestures in response to questions, reaching for objects, holding or touching objects in a manner dependent on the shape and size of the object, and pursuit eye movement or ocular fixation (12,13). Patients may evolve to the minimally conscious state following coma or the vegetative state. The most common causes of the minimally conscious state are acquired brain injury, neurodegenerative diseases, neurometabolic conditions, or congenital disorders (14). Survival is predicted more strongly by mobility than by the precise degree of awareness. Among 5073 children in the vegetative or minimally conscious states studied, 8 year survival was 65% for immobile minimally conscious patients, 81% for mobile minimally conscious patients, and 63% for patients in the vegetative state (15).
Recent studies have further blurred the distinction between the minimally conscious and vegetative states. Functional neuroimaging and electrophysiology studies have demonstrated that some patients considered to be in the vegetative state based on detailed examination and responsiveness testing actually demonstrate reproducible physiologic changes in response to tasks, indicating there may be some awareness despite the absence of behavioral signs of responsiveness (16–18). These findings have led to a recent shift toward the use of more neutral and descriptive terms (19,20). The vegetative state may be referred to as the unresponsive wakefulness syndrome. The minimally conscious state may be subdivided into the minimally conscious state plus (MCS+) if there are high-level behavioral responses, such as following commands or intelligible verbalizations, or the minimally conscious state negative (MCS−) if there are lower level behavioral responses, such as visual pursuit or contextually appropriate crying or smiling (19).
Akinetic mutism is an uncommon condition in which wakefulness and awareness are partially preserved, but there is extreme slowing or absence of bodily movement, reduced mental function, and loss of speech. This state may result from extensive bihemispheric disease and lesions involving the bilateral inferior frontal lobes, paramedian mesencephalic reticular formation, or the posterior diencephalon. Causes include tumors, bacterial and viral infections, and hydrocephalus. It may occur postoperatively following resection of posterior fossa tumors. Prognosis is dependent on etiology.
It is important to be aware of conditions with normal mental status that mimic coma since failure to recognize them will cause avoidable suffering. In these conditions, cognitive function is preserved and the electroencephalogram (EEG) is normal. The locked-in syndrome is a state of preserved consciousness and cognition with complete loss of voluntary motor functions (other than vertical eye movements and blinking). Cerebral cortical function is intact and EEG patterns are normal. The locked-in state is seen with lesions of the corticospinal and corticobulbar pathways at or below the pons (as in brainstem strokes). Vertical eye movements or blinking allow communication, such as answering yes/no questions. Some children with locked-in syndrome may show motor recovery (21). Similarly, neuromuscular disorders causing severe loss of cranial and limb movement may appear as coma but normal mental status can be demonstrated with careful testing. These include Miller-Fisher variant of Guillain-Barré syndrome, botulism, myasthenia gravis, and critical illness polyneuropathy. Psychogenic unresponsiveness may mimic coma.
Coma must also be distinguished from brain death, which is the permanent absence of all brain activity including brainstem function. The most recently published recommendations regarding brain death state that “determination of brain death in neonates, infants, and children relies on a clinical diagnosis that is based on the absence of neurologic function with a known irreversible cause of coma” (22). Patients must fulfill specific criteria, and many institutions have specific brain death protocols.
■ ANATOMY OF COMA
Wakefulness is maintained by the reticular activating system (RAS) while awareness is dependent on the cortex and subcortical connections. The RAS extends from the caudal medulla to the thalamus and basal forebrain. It receives input from all sensory pathways and projects to extensive areas of the cerebral cortex, thereby activating cortex and permitting feedback control to regulate incoming signals. The RAS may be partitioned into medial and lateral zones. The medial RAS zone has ascending axons emanating from the raphe nuclei, which regulate sleep cycles and utilize serotonin as their major neurotransmitter. Descending pathways regulate automatic motor functions including the automatic rhythms of breathing. The lateral RAS zone uses cholinergic and noradrenergic projections to the reticular nucleus of the thalamus to relay signals to the cortex, and this system is critical to maintaining wakefulness. A separate cholinergic pathway ascends through the hypothalamus and influences basal forebrain structures (including the limbic system) to influence conscious behavior, and lesions may result in akinetic mutism. A third noradrenergic pathway originates in the locus caeruleus and excites widespread areas of brain, mediating arousal and priming the brain to be activated by stimuli.
■ ENCEPHALOPATHY/COMA ETIOLOGIES
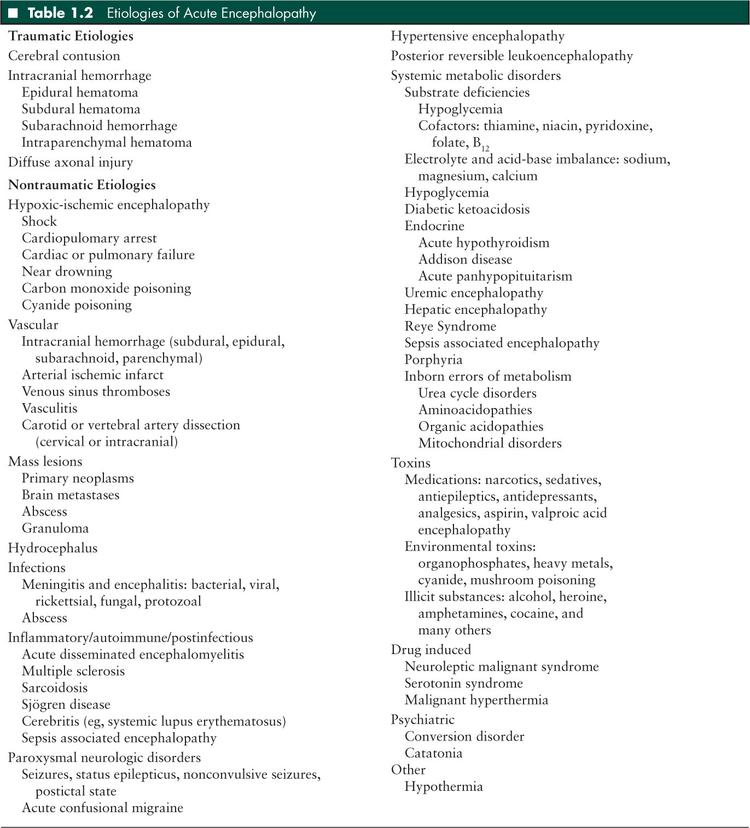
The causes of acute encephalopathy/coma in children are broad (Table 1.2). Multiple systems of categorization are possible. Etiology may be categorized as (1) traumatic or nontraumatic, (2) structural or toxic-metabolic, or (3) focal or diffuse. Nontraumatic subcategories include toxic-metabolic etiologies and structural abnormalities. Multiple interrelated etiologic factors may be present. For example, status epilepticus may occur in the setting of encephalitis, infection inducing a catabolic state may produce decompensation in a child with an inborn error of metabolism, and hyponatremia may accompany brain injury and contribute to cerebral dysfunction. Thus, identifying one etiology does not preclude consideration of other etiologies.
In a population-based study of 600,000 children experiencing 345 episodes of non-traumatic coma, the most common etiology was infection (38%), while intoxication, epilepsy, complications of congenital abnormalities, nontraumatic accidents (smoke inhalation, drowning), and metabolic causes each accounted for 6% to 10% of cases (1). Traumatic brain injury is the most common cause of coma in children, not only because trauma is common but also because it frequently leads to coma. Approximately 27% of patients with traumatic brain injury have an initial Glasgow Coma Score of less than 9 (4).
■ EVALUATION
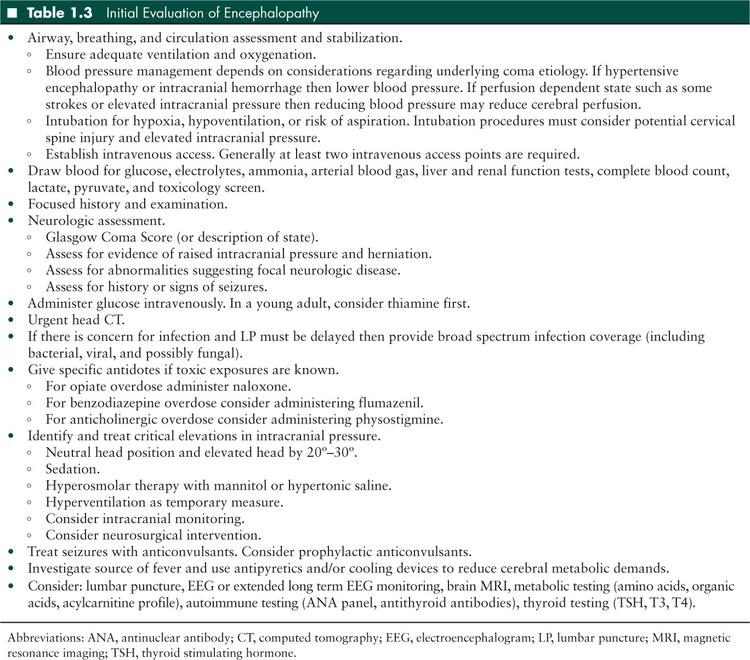
The evaluation of the encephalopathic or comatose child must be rapid, systematic, and comprehensive. In those cases where the cause is reversible, the neurologic effects may only be reversed if the cause is treated promptly. In the case of coma, systemic management including immediate life support must occur as etiology is being investigated to prevent development of secondary brain injury. An algorithm for initial evaluation of acute encephalopathy/coma is outlined in Table 1.3. A recent guideline for the evaluation and management of a child with decreased consciousness by the Pediatric Accident and Emergency Research Group of the Royal College of Paediatrics and Child Health and the British Association for Emergency Medicine (www.nottingham.ac.uk/paediatric-guideline) is based on extensive literature review and expert consensus and includes helpful flowcharts (23). Other reviews are also available (24–26).
History
Historical information may help identify the cause of encephalopathy and should include a detailed description of events leading up to the illness including timing of events, possible exposures, and initial symptoms (Table 1.4). Preceding somnolence or headache that progress suggests metabolic etiologies, toxin or medication exposures, infectious etiologies, hydrocephalus, or expanding mass lesions that may have been developing over time. In contrast, the sudden onset of illness without trauma suggests intracranial hemorrhage, seizure, cardiac arrhythmia producing hypoxic-ischemic encephalopathy, or ischemic stroke. A fluctuating course may occur with metabolic encephalopathy, seizures, or subdural hemorrhage. Head injury followed by a lucid period and then encephalopathy mandates a head computed tomography (CT) to evaluate for an epidural or expanding subdural hemorrhage. Focal symptoms followed by encephalopathy suggest a focal lesion that may have expanded, developed edema, or experienced intralesion hemorrhage.
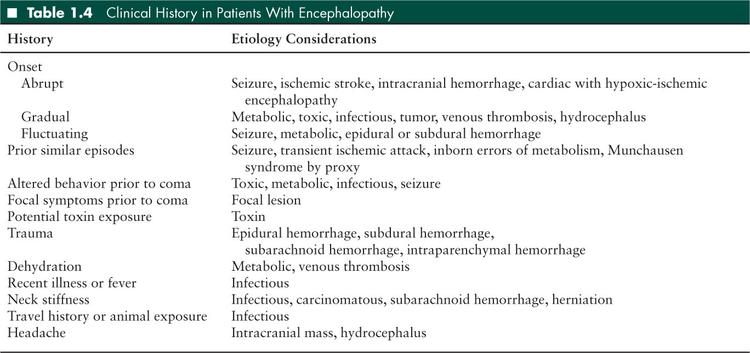
Eliciting a history of trauma and the mechanism of injury can direct investigation. Base of the skull fractures may compromise blood flow in the carotid artery, as in carotid artery dissection, producing serious middle cerebral artery ischemia. Preceding headache with positional changes or Valsalva maneuver implies increased intracranial pressure secondary to hydrocephalus or a mass lesion. Headache with neck pain or stiffness suggests meningeal irritation from inflammation, infection, or hemorrhage. Fever suggests infection, but its absence does not rule it out, particularly in infants under 3 months of age or immunocompromised children. Recent fever or nonspecific illness can signal autoimmune or postinfectious processes such as acute disseminated encephalomyelitis. A survey of medications and poisons in the child’s environment may suggest toxic ingestion. Travel history may explain exposure to infections prevalent in certain areas. Exposure to kittens in a patient with axillary or inguinal lymphadenopathy may be a clue to infection with Bartonella henselae induced cat scratch encephalopathy. Use of a heater or kerosene stove in an enclosed location may suggest carbon monoxide poisoning.
Past medical history may help elucidate etiology. Prior similar episodes can indicate transient ischemic attacks, recurrent ingestion, or Munchausen syndrome by proxy. Multiple episodes of encephalopathy or coma also raise a question about seizures or an inborn error of metabolism, especially if there is also history of developmental delay or other neurologic abnormalities. Cardiac disease raises the possibility of dysrhythmia or cardiac failure leading to hypoxic-ischemic encephalopathy, brain abscess, or stroke. A diagnosis of diabetes may suggest hypoglycemia or diabetic ketoacidosis. Weight changes, recent darkening of the skin, or other constitutional abnormalities may suggest endocrine dysfunction. Prior recurrent infections, known immunodeficiency, or use of immune suppressing medications may lead to consideration of infectious etiologies. A history of uncontrolled hypertension may suggest posterior reversible encephalopathy syndrome.
Physical Examination
The general physical examination should focus on identifying the etiology and complications that may produce secondary neurologic injury.
Encephalopathy, Coma, and Consciousness Rating Scales
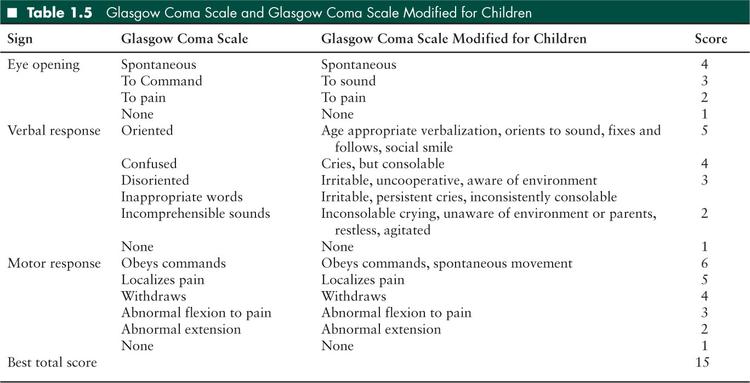
A detailed description of the mental status, indicating what the child can and cannot do, is the ideal method for relaying detailed information to other providers and detecting changes over time. There is also value in including numerically scored rating scales of consciousness level, which provide objective description of a patient’s consciousness and a tool for tracking the condition over time and conveying information quickly to other caregivers. The most widely used instrument is the Glasgow Coma Scale (GCS) which was initially developed to evaluate adults with head injury (27). Pediatric adaptations to the GCS, which are more developmentally appropriate for infants and children, include the Pediatric Coma Scale, the Children’s Coma Scale, and the GCS Modified for Children (Table 1.5) (28–30). The GCS and the pediatric adaptations categorize the patient based on measures of verbal response, eye opening, and movement. The GCS Modified for Children yields a 3 to 15 score based on the best response of the 3 categories.
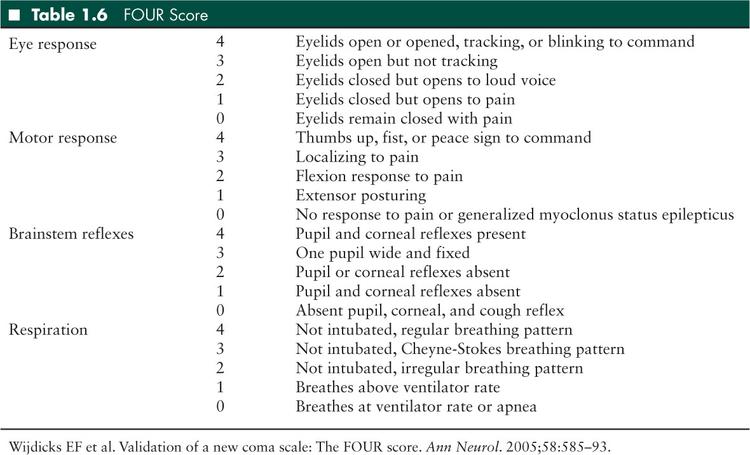
In response to limitations of the GCS, the FOUR score was recently developed for use in adults with coma (31). Each of 4 functional categories (eye response, motor response, brainstem reflexes, and respiration) receives a score of 0 (nonfunctioning) to 4 (normal functioning) (Table 1.6). Some differences from the GCS score include assessment of eye tracking in the eye response category, assessment of response to pain, ability to follow simple commands, the presence of generalized myoclonic status epilepticus in the motor response category, elimination of verbal response from the scale, and addition of brainstem reflex and respiratory categories (31). The FOUR score has proven useful in adults in the medical intensive care unit (ICU) (32) and after resuscitation from cardiac arrest (33). One study has evaluated the interrater reliability and predictive value of the GCS Modified for Children and FOUR score in critically ill children. In a study of 60 children aged 2 to 18 years in an ICU with both traumatic and nontraumatic brain injury, the FOUR score had better interrater reliability than the GCS Modified for Children (excellent for FOUR score and good for GCS) and both predicted outcome similarly (34). While many coma scoring systems exist (35), further validation of these tools is needed in children.
Vital Signs
Hypertension may cause encephalopathy or result from another condition that is causing altered mental status. Primary or secondary hypertension may cause hypertensive encephalopathy. Primary hypertensive encephalopathy is suggested by a history of hypertension or renal disease, or by preceding headache, visual complaints, or seizures. Hypertension may occur with Cushing syndrome, thyrotoxicosis, pheochromocytoma, drug overdose (cocaine, amphetamine, phencyclidine), renal disease (such as acute glomerulonephritis or chronic renal failure), medication exposure (such as immunomodulatory and chemotherapeutic drugs), and, rarely, essential hypertension. Importantly, in critically ill children, hypertension can be a physiologic response to elevated intracranial pressure that functions to maintain cerebral perfusion pressure. Differentiating between reactive/compensatory hypertension and a primary hypertensive encephalopathy may be difficult but is crucial in determining how to manage blood pressure. If hypertension is a response to elevated intracranial pressure, then acutely lowering blood pressure may worsen the neurologic injury by reducing cerebral perfusion. Hypertension, bradycardia, and irregular respiration (Cushing triad) is an ominous sign of elevated intracranial pressure and impending brain herniation. Management may require urgent measures to lower intracranial pressure such as hyperventilation, hyperosmolar therapy, and neurosurgical therapy.
Hypotension may cause encephalopathy or coma as a result of poor cerebral perfusion and associated diffuse or watershed hypoxic-ischemic injury. It may result in worse outcome in encephalopathy due to other causes. Hypotension may result from sepsis, cardiac dysfunction (which may be secondary to severe neurologic injury in neurogenic stunned myocardium), systemic hemorrhage, intracranial hemorrhage in neonate/infant, toxic ingestion, adrenal insufficiency, or hypothyroidism.
Tachycardia may occur with hypovolemic shock (due to dehydration or systemic hemorrhage), cardiogenic shock, sepsis, pain, toxin exposure (stimulants such as amphetamines, cocaine, nicotine, and caffeine), malignant hyperthermia, anemia, heart failure, hyperthyroidism, pheochromocytoma, or pulmonary embolism. Bradycardia may occur with intracranial hypertension, cardiac disease, hypothermia, toxin exposure (sedating drugs), uremic coma, or myxedema coma.
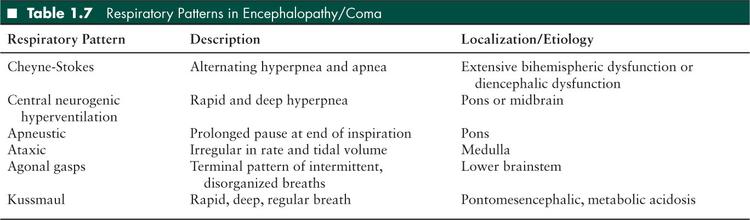
Abnormalities in respiratory rate and pattern of breathing may indicate pulmonary disease, acid-base derangement, or nervous system dysfunction. Tachypnea may occur with a primary abnormality of respiration (eg, asthma, pneumonia, or pulmonary embolism) or acidosis (eg, uremia or ketoacidosis). Cheyne-Stokes respiration describes a rhythmic and cyclic pattern of accelerating hyperpnea followed by decelerating respiratory rate and/or apnea. It is a nonspecific pattern seen with extensive bihemispheric cerebral dysfunction, diencephalic (thalamic and hypothalamic) dysfunction, or cardiac failure. Central neurogenic hyperventilation is characterized by rapid and deep hyperpnea and is caused by pontine or midbrain tegmental lesions. Apneustic breathing is characterized by prolonged inspiration, a few second pause, and then expiration. It is caused by damage to respiratory centers in the mid or lower pons. Apneusis also occurs with basilar artery occlusion (leading to pontine infarction), metabolic changes, or meningitis. Ataxic breathing is completely irregular in rate and tidal volume and occurs with damage to the reticular formation of the dorsomedial medulla. Kussmaul breathing refers to deep, rapid, and regular breaths and occurs with pontomesencephalic lesions or metabolic acidosis. Agonal gasps represent a terminal respiratory pattern and indicate damage to the bilateral lower brainstem (6). Respiratory patterns are summarized in Table 1.7.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


