CHAPTER 27 Anti-Reflux Procedures
Step 1: Surgical Anatomy
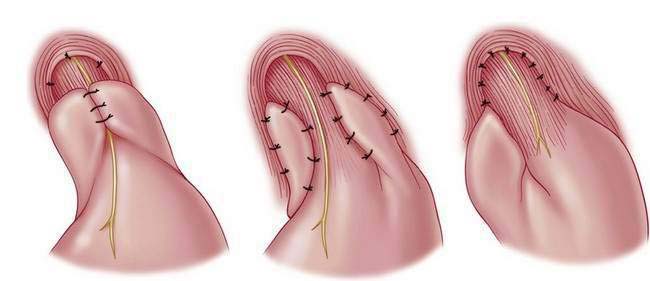
♦ In children, Nissen (360 degrees), Toupet (270 degrees) posterior, and Thal (270 degrees) anterior wrap are options. We typically advocate a laparoscopic Nissen fundoplication with or without concomitant gastrostomy tube placement when indicated and feasible (Fig. 27-1).
Step 2: Preoperative Considerations
♦ Gastroesophageal reflux in the child is largely a clinical diagnosis based on one or more conditions (e.g., emesis, chronic cough, wheezing, aspiration pneumonia) and their sequelae (e.g., esophagitis, nutritional failure or growth retardation, apnea, sudden infant death syndrome, or acute life-threatening events).
♦ The clinical diagnosis is supported by pH probe studies. A cookie-swallow study can be helpful to assess penetration. On esophagram, most infants appear to have reflux, limiting the utility of this test. We routinely perform an upper gastrointestinal (GI) series to rule out malrotation before operation, but this can also be ascertained laparoscopically by determining the location of the ligament of Treitz, cecum, and small bowel when the upper GI is equivocal. Some advocate a gastric emptying study. An esophagogastroscopy with biopsy is not imperative but can be helpful for identification of reflux stigmata. The liberal use of Nissen fundoplication in neurologically impaired children appears to be advantageous. Antibiotic prophylaxis is achieved by administering a first-generation cephalosporin (e.g., cefazolin) 30 minutes before surgical incision and continued for 24 hours postoperatively.
♦ There are no absolute contraindications to an attempt at laparoscopy. However, extensive adhesions from prior surgery (including open Nissen or gastrostomy), ventilator or hemodynamic instability (poor tolerance of CO2 insufflation or pressure), marked visceral dilation (often from excessive preintubation bagging or preceding ileus), hepatosplenomegaly, existing ventriculoperitoneal shunt or baclofen pump, and scoliosis can make a laparoscopic approach more challenging.
♦ There are important differential considerations for infants who weigh less than 5 kg compared with a larger child or adolescent. Small infants are best served by using 3-mm instruments and liver retractor, whereas 5-mm instruments are more suitable for a larger child. Of additional consideration is the larger child with scoliosis, magnetic resonance cholangiopancreatography, or additional hardware (e.g., baclofen pump), which can make a routine case more technically demanding with respect to port placement and overall operative strategy (Fig. 27-2).
♦ An inventory of equipment follows (some shown in Fig. 27-3): trocars (5 mm for right upper quadrant liver port and umbilical camera), “radially” expanding sheaths and trocars, scopes (4 mm, 30 degrees;, 5 mm, 30 degrees; and 10 mm, 30 degrees), graspers (Maryland or Duckbill), needle drivers, hook cautery (alternative Harmonic scalpel), fundus grasper, liver retractor and holder), suture, suction irrigator, video monitors, and laparoscopic tower.
Step 3: Operative Steps
Anesthetic Induction
♦ For port-site placement, 0.25% Marcaine (1 mL/kg) is administered before each incision. Intubation is performed in standard fashion after orogastric tube decompression. For larger children, tapered Maloney dilators (20 to 44 French) may be placed into the esophagus.