Chapter 705 Animal and Human Bites
Epidemiology
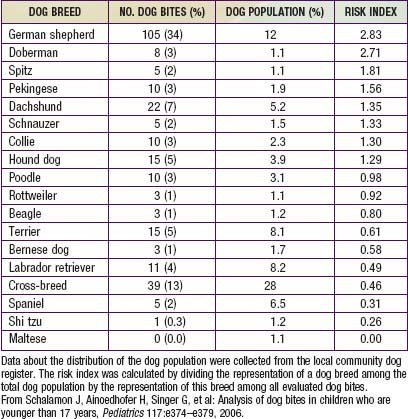
During the past 3 decades, there have been approximately 20 deaths per year in the USA from dog-inflicted injuries; 65% of these occurred in children younger than 11 yr. The breed of dog involved in attacks on children varies; Table 705-1 depicts the risk index by breed from one study of 341 dog bites. Rottweilers, pit bulls, and German shepherds accounted for more than 50% of all fatal bite-related injuries. Unaltered male dogs account for approximately 75% of attacks; nursing dams often inflict injury to humans when children attempt to handle one of their puppies.
Complications
The rate of infection after rodent bite injuries is not known. Most of the oral flora of rats is similar to that of other mammals; however, approximately 50% and 25% of rats harbor strains of Streptobacillus moniliformis and Spirillum minus, respectively, in their oral flora. Each of these agents has the potential to cause infection (Chapter 705.1).
Common causes of soft tissue bacterial infections after dog, cat, or human bites are noted in Table 705-2. High risk for infection after a bite is associated with wounds in the hand, foot, or genitals, penetration of bone or tendons, human or cat bites, delay in treatment longer than 24 hr, presence of foreign material, immunosuppression (asplenia), and crush or deep puncture wounds.
Table 705-2 MICROORGANISMS ASSOCIATED WITH BITES
DOG BITES
CAT BITES
HERBIVORE BITES
SWINE BITES
RODENT BITES—RAT BITE FEVER
PRIMATE BITES
LARGE REPTILE (CROCODILE, ALLIGATOR) BITES
Adapted from Perkins Garth A, Harris NS: Animal bites (website). http://emedicine.medscape.com/article/768875-overview. Accessed December 3, 2010. Reprinted with permission from eMedicine.com, 2009.
Treatment (Table 705-3)
Table 705-3 PROPHYLACTIC MANAGEMENT OF HUMAN OR ANIMAL BITE WOUNDS TO PREVENT INFECTION
| CATEGORY OF MANAGEMENT | MANAGEMENT |
|---|---|
| Cleansing | Sponge away visible dirt. Irrigate with a copious volume of sterile saline solution by high-pressure syringe irrigation.* |
| Do not irrigate puncture wounds. Standard precautions should be used. | |
| Wound culture | No for fresh wounds, unless signs of infection exist. |
| Yes for wounds more than 8-12 hr old and wounds that appear infected.† | |
| Radiographs | Indicated for penetrating injuries overlying bones or joints, for suspected fracture, or to assess foreign body inoculation. |
| Debridement | Remove devitalized tissue. |
| Operative debridement and exploration | Yes for one of the following conditions: |
| Wound closure | Yes for selected fresh, nonpuncture bite wounds (see text) |
| Assess tetanus immunization status | Yes |
| Assess risk of rabies from animal bites | Yes |
| Assess risk of hepatitis B virus infection from human bites | Yes |
| Assess risk of human immunodeficiency virus from human bites | Yes |