Introduction
Androgen excess includes a vast spectrum of clinical presentations and symptoms. The key to the differential diagnosis and treatment of androgen excess states is to differentiate the patient who presents with hirsutism from the patient who presents with virilization (Box 92.1). A basic understanding of androgen production and actions allows the clinician to make the appropriate diagnosis.
Androgens are produced in the ovary and the adrenal gland, and androgen precursors are converted to androgens in the periphery. The ovary produces testosterone, androstenedione, and dehydroepiandrosterone (DHEA). The adrenal gland produces androstenedione, DHEA, and dehydroepiandrosterone sulfate (DHEAS). More than 90% of DHEAS is derived from the adrenal. Regardless of source of origin, androstenedione and DHEA are converted in the periphery to testosterone. Testosterone is further metabolized to dihydrotestosterone (DHT) and its metabolite, 3α-androstanediol glucuronide (3α-diolG), at the receptor sites in the skin and genitalia. Total testosterone production in the woman is 0.35 mg/day, with the majority arising from peripheral conversion.
Most circulating testosterone (85%) is bound to sex hormone-binding globulin (SHBG) and is considered biologically inactive. Biologically active testosterone is mainly albumin associated (10–15%) and “free” (1–2%). Non-SHBG-bound testosterone is elevated in 60–70% of hirsute women. Hypothyroidism, obesity, hyperinsulinemia, and hyperandrogenism are associated with decreased SHBG leading to elevated “free” testosterone. Hyperthyroidism and estrogen increase SHBG and decrease free testosterone levels. In hirsute women there is an excellent correlation between total and non-SHBG-bound testosterone.
Androgens exert their actions when bound to their appropriate receptors. Areas of the body where androgen receptors are present are considered to be androgen sensitive.
Hirsutism is increased terminal hair growth usually in areas where it does not normally occur but which contain androgen receptors. Terminal hairs are coarse, long, and pigmented and normally grow in the pubis, scalp, axillae, eyebrows, legs, and arms. Hirsutism may result from either elevated circulating androgens or increased sensitivity of the pilosebaceous unit to androgens. Androgen stimulation of the hair follicle results in transformation of fine, soft, unpigmented vellus hairs into the coarser terminal hairs. Hirsutism is defined as excessive terminal hair growth over an androgen-sensitive area of the body where hair growth is normally minimal or absent. These areas include the face, chest, areola, lower abdomen, inner thighs, and back. However, what may be considered excessive growth in one culture or family may not be considered excessive in another. The amount of hair is related to the potency of the circulating androgens, quantity of ciculating free androgens, duration of exposure, sensitivity of the hair follicle, and density of the hair follicle.
Box 92.1 Differential diagnosis of hirsutism and virilization
Ovarian
PCOS
hyperthecosis
neoplasms
Adrenal
CAH
neoplasms
Cushing’s syndrome
Idiopathic
Drugs
anabolic (testosterone/adrenal) steroids
danazol
19-norsteroid derivative progestogens
Other endocrine disorders
acromegaly
menopause
thyroid disease
In general, hirsutism is gradual in onset and often presents as a cosmetic or infertility complaint. Hirsutism is usually associated with normal or minimally elevated levels of serum androgens. However, there are many periods in a woman’s life, such as pregnancy, puberty, and after menopause, when hair may appear at an accelerated rate as a result of physiologic changes in circulating sex steroids.
Hirsutism should be differentiated from hypertrichosis, which is a diffuse increase in terminal and vellus hairs that can occur all over the body. Hypertrichosis is a reversible side effect of phenytoin or minoxidil, occurs occasionally with anorexia nervosa, and rarely is a congenital X-linked disorder.
Virilization is the masculinization of a woman. In addition to hirsutism, these women present with temporal hair recession, acne, deepening of the voice, malodorous sweat, clitoral enlargement, atrophy of the breasts, increased muscle mass, loss of female body contours, and amenorrhea. Signs of virilization usually appear over a relatively short period of time and are indicative of serious endocrine disease. Virilization is associated with a marked increase in circulating androgen levels.
History and physical examination
A history is obtained of the age of onset of hair growth, the amount, duration, rate, and distribution. Symptoms of virilization, menstrual history and infertility, drug history, and the co-existence of other medical diseases are also uncovered. The family history of hirsutism or other endocrine disorders aids in the diagnosis of familial or genetic forms of hirsutism.
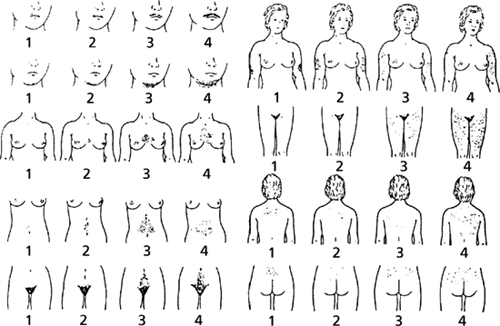
Physical examination will reveal the severity of the hirsutism, signs of virilization, and other associated endocrine disorders. The Ferriman–Gallwey scoring system assesses the severity of hirsutism and is used to analyze response to treatment. A modified Ferriman–Gallwey, as shown in Figure 92.1, scores the degree of hirsutism from nine androgen-sensitive body sites including chin, upper lip, mid-line hair between the breasts, upper and lower abdomen. A score of 8 or more is considered abnormal. It is important to consider racial and ethnic differences when determining what is truly excessive hair growth. The Ferriman–Gallwey scale was developed in England and a traditionally “normal” score is based on white British women. In research settings, the degree of hirsutism and response to therapy are often determined by shaving a specific area and either counting the number of hairs or weighing the hair.
Figure 92.1 Hirsutism scoring from 1 to 4 from nine body sites. Reproduced with permission from Ferriman D, Gallwey JD. Clinical assessment of body hair in women. J Clin Endocrinol Metab 1961; 21: 1440-1447. ©The Endocrine Society.
Signs of virilization include high scores on the Ferriman–Gallwey system, clitoromegaly, increased muscularity and/or male body habitus, male-pattern balding, and deepening of the voice. Signs suggestive of other endocrine disorders, such as Cushing’s syndrome (central obesity, hypertension, striae, easy bruising) and congenital adrenal hyperplasia (CAH) (abnormal blood pressure, short stature) are noted. Signs of metabolic syndrome include abdominal obesity (waist circumference >88 cm (>35 inches)) and an elevated blood pressure.
Serum testosterone and DHEAS levels are the initial screening tests in the work-up of the hirsute woman. Testosterone levels are primarily derived from the ovary and thus serve as a marker for excess ovarian androgen production. DHEAS levels are a direct reflection of excess androgen production by the adrenal gland. A testosterone level greater than 200 ng/dL is suggestive of an ovarian tumor. Definitive diagnosis is made with imaging studies. A DHEAS level greater than 8 μg/dL suggests an adrenal tumor. Lower yet abnormal values of these hormones may indicate an exogenous or iatrogenic cause, the presence of idiopathic androgen excess, polycystic ovarian syndrome (PCOS), stromal hyperthecosis, CAH or Cushing’s syndrome.
Screening for adult-onset CAH is accomplished by measuring 17-hydroxyprogesterone (17-OHP) concentrations. Normal baseline 17-OHP should be less than 200 ng/mL if measured first thing in the morning. Levels between 200 and 800 ng/mL require ACTH testing. Cortisol, 11-deoxycorticol, and 17-OHP are measured in serum before and 30 and 60 minutes after the administration of 250 μg of synthetic ACTH. The blood sample should be obtained during the follicular phase of the cycle. Patients with CAH demonstrate a disproportional increase in 17-OH progesterone compared to cortisol levels. Baseline levels of 17-OHP above 800 ng/mL are diagnostic of a 21-hydroxylase deficiency.
Collection of urine for measurement of 24-hour urinary free cortisol and creatinine is the preliminary screening test for the diagnosis of Cushing’s disease. Measurement of fasting glucose and insulin levels is indicated in the work-up of those patients who may be insulin resistant.
Idiopathic hirsutism
Idiopathic hirsutism classically presents as hirsutism in a patient with regular, ovulatory menstrual cycles and normal circulating androgen levels. Idiopathic hirsutism is a diagnosis of exclusion. Patients with idiopathic hirsutism present either with mildly elevated or normal testosterone levels. Many patients with idiopathic hirsutism have elevated levels of 3α-androstanediol-glucuronide (3α-diolG), a marker of peripheral androgen activity. Specifically, 3α-diolG is a marker of 5α-reductase activity in the pilosebaceous unit. This is the enzyme which converts testosterone to the highly androgenic DHT. Although androgens are the main regulators of 5α-reductase activity, another major factor is the genetic expression of this enzyme. If testosterone and DHEAS are normal and 3α-diolG is elevated, a peripheral disorder (i.e. abnormality at the psu unit) is suggested.
Polycystic ovarian syndrome
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


