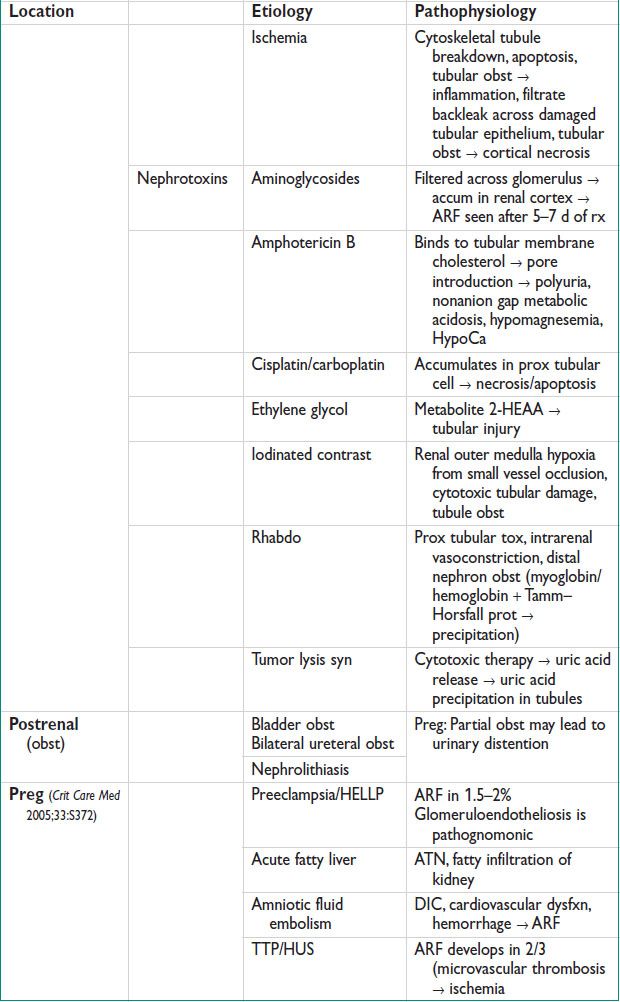
Clinical Findings & Exam
• Uremia, oliguria/anuria, hematuria
• Prerenal: Tachy, dry mucous membranes, orthostatic HoTN
• Intrarenal: Pulm hemorrhage, palpable purpura → vasculitis + glomerulonephritis, livedo reticularis → atheroembolic dz, limb ischemia → rhabdo
• Postrenal: Flank pain which radiates to groin, suprapubic pain
Diagnostic Workup
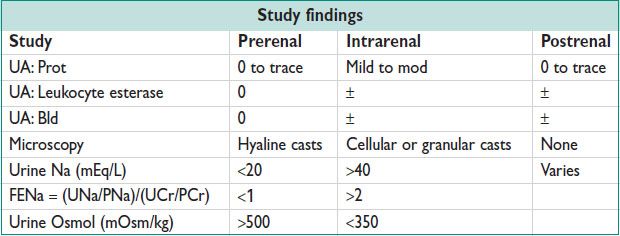
Subsequent Workup
• Renal bx: Consider when etiology is unk. 5% complication rate (perirenal hematoma, gross hematuria). Preg: Consider pts <28 w w/ ARF of uncertain etiology when results will change mgmt (Am J Perinatol 2008;25:385)
Treatment
• Correct underlying factors, remove renal toxins, adjust dosing of renally cleared meds. Prevent/treat infxn
• Fluid mgmt: Goal = adequate hydration to reverse preischemic change
• HyperK → polystyrene sulfonate
• Metabolic acidosis → sodium bicarbonate
• RRT (JAMA 2008;299:793)
For ARF refrac to medical mgmt, as evidenced by metabolic acidosis, hyperK, hypervolemia, etc. Mode: IP, intermittent hemodialysis, continuous RRT.
Continuous RRT: Slower solute clearance/min, continuous anticoagulation
Use in Preg:
Symptomatic uremia (changes in mental status, pericarditis, neuropathy)
HyperK not corrected by medical mgmt
Metabolic acidosis
Vol overload
CHRONIC RENAL FAILURE
Definition and Epidemiology (MMR 2007;56:161)
• CKD = abn kidney fxn + progressive decline of estimated GFR for >3 mo
• CRF: Irreversible nephron number reduction
• ESRD: GFR <15 mL/min per 1.73 m2 OR need for dialysis &/or xplant
• Prevalence of CKD in US: 16.8% of adults ≥ age 20 (11.1% stages 1–2, 5.8% stages 3–5), & increased prevalence w/ comorbidities such as DM (40.2%), cardiovascular dz (28.2%), & HTN (24.6%)
Etiology
• Glomerular dz: Diabetes, systemic infxn, autoimmune dz
• Vascular dz: HTN, ischemia, atherosclerosis, vasculitis, thromboembolic
• Tubular/interstitial dz: Urinary tract stones, infxn, obst, nephrotoxic meds
Pathophysiology
• Initiating mechanisms: Specific to etiology of CKD
• Progressive mechanisms: Increased renal bld flow/pres → renin–angiotension axis stimulation → nephron hyperfiltration & hypertrophy → glomerular distortion, sclerosis, permanent damage to nephrons → reduction in nephron number
• Failure of renal excretion → accum of toxins (including Cr, urea → uremic syn). Failure of other renal functions → anemia, abn metabolism, fluid/electrolyte imbalance, hormone regulation (glucagon, insulin, Vit D, sex hormones, parathyroid hormone). Progressive inflammation (elevated C reactive prot + acute phase reactants).
Clinical Manifestations
• Edema (from nephrotic syn), fatigue (from anemia), decreased appetite → malnut, inability to perform activities of daily living (uremic syn).
• Preg (CJASN 2011;6:2587): 3 factors correlate w/ ↑ complications: Proteinuria, decreased GFR, HTN
Maternal complications: Gestational HTN, preeclampsia/eclampsia, nephrotic syn, maternal death (higher incid w/ lupus nephropathy)
Fetal complications: Preterm birth, IUGR, IUFD, neonat death
Physical Exam
• Most pts are asymptomatic until mod or sev renal failure develops
• Findings may include periph edema, pericardial friction rub (in presence of uremic syn), sensory neuropathy (evid of end-organ damage)
Diagnostic Workup/Studies
• GFR (mL/min per 1.73 m2) = 1.86 × (PCr) – 1.154 × (age) – 0.203
PCr = serum Cr; multiply by 1.21 for AAs or 0.742 for women
• GFR peak = 120 mL/min per 1.73 m2 btw age 20 & 30 (lower for women)
• GFR then declines 1 mL/min per 1.73 m2 per year
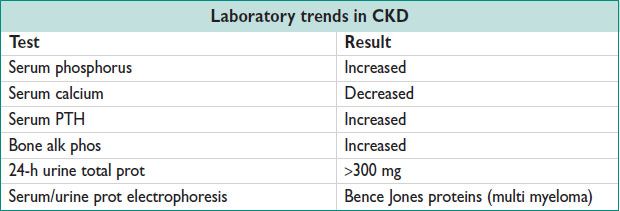
Stages of CKD GFR (mL/min per 1.73 m2)
• Stage 1: ≥90 + kidney damage (proteinuria, abn renal imaging)
• Stage 2: 60–89
• Stage 3: 30–59
• Stage 4: 15–29
• Stage 5: <15
Imaging
• Renal US (preferred modality in Preg)
CKD: Small kidneys bilaterally
Polycystic kidney dz: Cystic, enlarged kidneys
>1 cm discrep in length: Developmental abnormality, arterial insufficiency which affects one kidney more
• Voiding cystogram: To evaluate for reflux nephropathy
• CT, MRI: Avoid IV dye if poss in Preg
• Renal bx: Should be avoided during Preg
• Serial renal fxn measurements (to differentiate acute vs. subacute vs. CKD)
Treatment and Medications
• Potassium sparing meds: ACE inhibitors, ARB, spironolactone, eplerenone, amiloride, triamterene
• Dietary adjustments (decreased salt intake)
• HTN control (Lancet 2005;365:331)
Goal = 130/80 (125/75 in pts w/ diabetes & proteinuria > 1 g/24 h)
Reduce intraglomerular HTN to slow nephron injury progression
• Renal replacement therapy: IP vs. intermittent hemodialysis vs. continuous RRT. Initiate when GFR = 10 mL/min per 1.73 m2
• Preg: 24-h urine total prot in the 1st trimester + HTN control (BB, CCB, hydralazine, clonidine) + Serial USs for fetal growth + antepartum testing: Initiate btw 28 & 32 w. Avoid ACE inhibitors/ARBs.
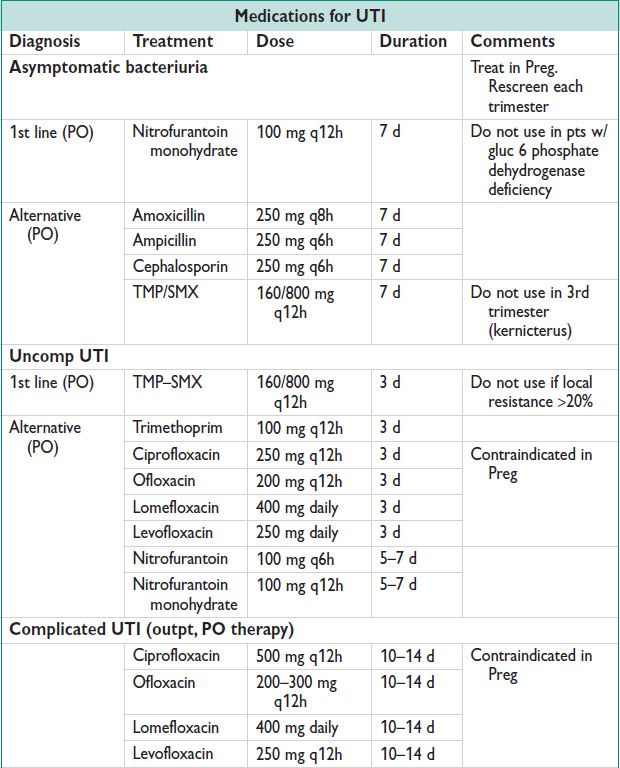
URINARY TRACT INFECTION (UTI)
Definitions
• Asymptomatic bacteriuria: 10000–100000 CFU/mL in urine culture (Obstet Gynecol 2005;106:1085)
• UTI: ≥100000 CFU/mL in urine culture w/ or w/o sx
• Uncomp: Healthy female w/ nml urinary tract fxn
• Complicated: UTI+ one of the following: Urologic abnormality, urinary calculi, FB (catheter), DM, Preg, spinal cord injury
• Recurrent UTI: 2 Uncomp UTIs in 6 mo or 3 positive cx w/i the preceding 12 mo (Obstet Gynecol Clin North Am 2008;35)
Epidemiology
• 50%  will have a UTI in their lifetime; 10%
will have a UTI in their lifetime; 10%  will have a recurrent UTI by age 70
will have a recurrent UTI by age 70
• Asymptomatic bacteriuria in Preg: 20–30× increased risk of pyelo
Etiology
• Escherichia coli = 75–95% (NEJM 2012;366:1028), Proteus (can cause renal calculi). Klebsiella, Enterobacter, Pseudomonas, Staphylococcus saprophyticus (common in young women)
Pathophysiology
• Ascending infxn: Vagina → urethra → bladder
• E. coli: Virulence factors P fimbria, S fimbria, Type 1 fimbria → ↑ uroepithelial/vaginal cell binding, ↑ resistance to host phagocytosis, ↑ resistance to bactericidal activity
Clinical Manifestations and Exam
• Dysuria, increased urgency, increased urinary frequency, suprapubic pain
• Suprapubic tenderness to palpation
• Pyuria, urethral tenderness (seen w/ urethritis)
Diagnostic Workup/Studies
• UA: Leukocyte esterase or nitrites: 75% sensitive, 82% specific (NEJM 2003;349:259); WBC ± RBC; bacteria on gram stain
• Urine culture: ≥100000 CFU/mL
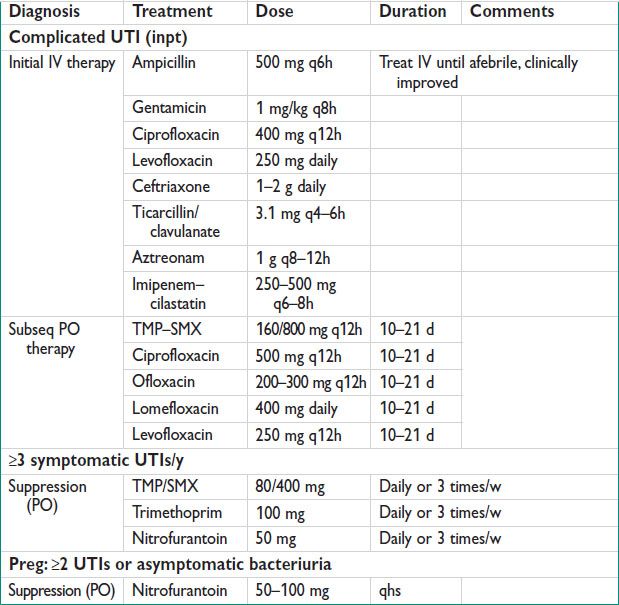
Treatment
PYELONEPHRITIS
Definition
• Infxn of renal pelvicalices/parenchyma from ascending bladder infxn or renal bacteriuria. Clinical syn defined by flank pain, fevers, chills.
Epidemiology
• 23/10000 women ages 15–34 (NEJM 2012;366:1028)
• 1–2% of pregnancies, >50% present in the 2nd trimester (Obstet Gynecol 2005;106:1085)
• Untreated asymptomatic bacteriuria in Preg → 1/4 will develop pyelo
Etiology
• Same as for UTIs (above). Most are E. coli.
Pathophysiology
• Risk factors: Same as for UTI (see UTI section)
• ARDS: IV antibiotic therapy → endotoxin release 24–48 h later → damage to alveolar capillary membranes
• Preg complications
Increased risk of preterm labor if pyelo is not aggressively treated
Pulm insufficiency: Increased risk if temperature >103°F, tachy >110 bpm, gestational age ≥20 w
Clinical Manifestations and Exam
• Chills, fever, flank pain, dysuria, urinary frequency/urgency
• Costovertebral angle tenderness
Diagnostic Workup/Studies
• Urinalysis
• Urine culture w/ susceptibilities
• If no resp to initial therapy, consider bld cx
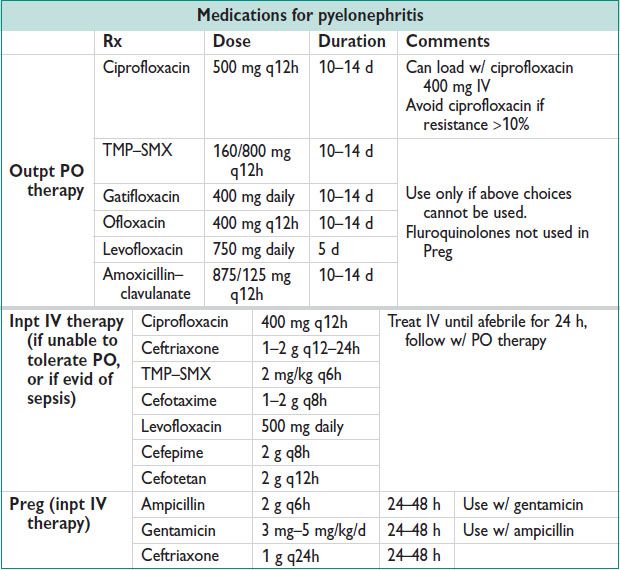
Treatment and Medications
• Inpt admission is recommended for all women w/ pyelo during Preg (Obstet Gynecol 2005;106:1085)
IV hydration to maintain adequate urine output
Acetaminophen: Hyperthermia can be teratogenic in 1st trimester
IV therapy 24–48 h (avoid fluoroquinolones), follow w/ oral therapy 10–14 d
• Suppression therapy for remainder of Preg: Nitrofurantoin 100 mg PO daily
• Rpt urine culture each trimester
Treatment
NEPHROLITHIASIS
Definition and Epidemiology
• Calcium-based: Calcium oxalate, calcium phosphate (80%) (NEJM 2010;363:954)
• Noncalcium-based: Uric acid, cystine, struvite (may form staghorn calculi)
• 10% of the US pop will have one kidney stone in lifetime (J Urol 2012;188:130)
• Preg: Btw 1/200 to 1/1500 women have symptomatic nephrolithiasis (Cur Op Uro 2010;20:174)
Pathophysiology
• Increased excretion rate or increased water conservation → supersaturation of urine w/ insoluble substances → crystal formation → crystal aggregation into stone(s)
• Stones become symptomatic when entering ureter or occluding uteteropelvic junction
Clinical Manifestations
• Flank pain (episodic, may radiate to abd), nausea, vomiting, hematuria, difficulty finding a comfortable position
Diagnostic Workup/Studies
• CT w/o contrast = imaging modality of choice
• Renal US
• Abdominal radiograph (KUB): Only + if radio-opaque stones
• Preg: Renal US = preferred modality
• Recurrent symptomatic nephrolithiasis: Evaluate poss etiologies
Serum: Calcium, uric acid, electrolytes
Urine: pH, vol, calcium, citrate, oxylate, 24-h urine collection (2 occasions)
Treatment and Medications
• Conservative mgmt: Hydration, pain control (most stones smaller than 0.5 cm pass spontaneously)
• Medical mgmt: Alpha-1 blockers to ↑ motility
• Active intervention req for persistent pain, progressive obst, infxn, solitary kidney obst (J Urol 2012;188:130)
Shock wave lithotripsy: May require multi treatments
Semirigid ureteroscopy: Higher stone free rate after one rx, fewer retreatments needed. Improved success w/ distal ureteral stones.
Percutaneous nephrolithotomy: Most invasive. Use for large stone burden, renal stones.
• Preg: (Cur Op Uro 2010;20:174)
Temporary drainage: Ureteral stent or percutaneous nephrostomy (risk of infxn, bacteriuria, migration/dislodgement)
Definitive rx: Ureteroscopy is preferred
Avoid shock wave lithotripsy in Preg (increased risk of miscarriage, congen malformations, abruption)
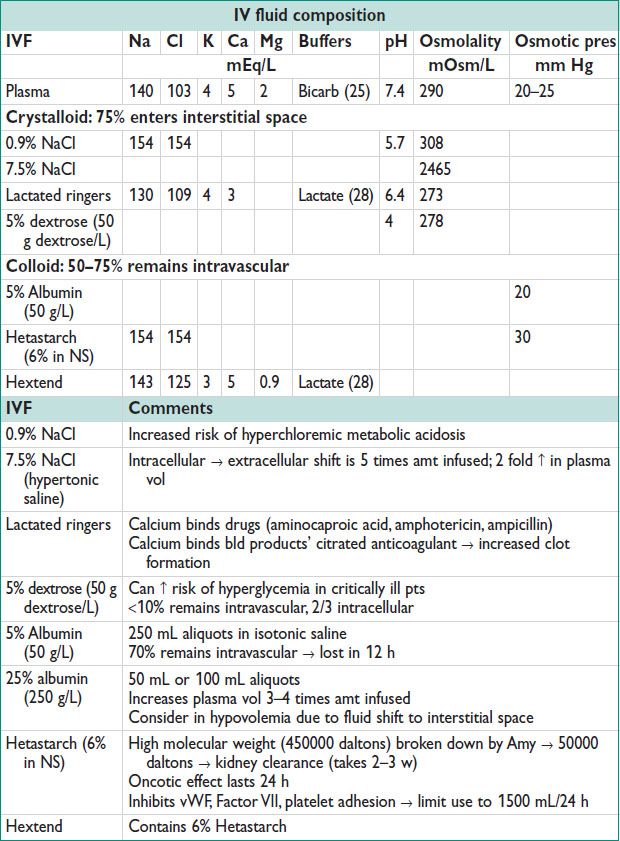
FLUIDS AND ELECTROLYTES
Hyperkalemia
• Definition: Serum potassium (K+) >5.5 mEq/L
• Clinical manifestations:
ECG changes (seen when K+ >6 mEq/L): Peaked T waves → 1° heart block → complete heart block → Vfib → asystole
Abdominal pain, myalgias, diarrhea, flaccid paralysis
• Dx:
Rule out pseudohyperkalemia
Urine K+
>30 mEq/L → transcellular shift
<30 mEq/L → impaired renal excretion
• Rx & meds: (J Int Care Med 2005;20:272)
Continuous telemetry
Sodium polystyrene sulfonate (Kayexalate): Cation exchange resin binds K+ → fecal excretion
PO: 30 g diluted in 50 mL of 20% sorbitol, rpt q2h
Rectal: 50 g diluted in 200 mL of 20% sorbitol, rpt q2h
Do not use in pts w/ bowel obst, ileus, bowel ischemia
If ECG changes are present
Calcium gluconate: 10 mL of 10% (1 ampule): IV push over 2 min. Rpt in 5 min.
Calcium chloride: 10 mL of 10% (1 ampule): Use in pts w/ circulatory compromise. 3× more calcium than calcium gluconate → improved cardiac contractility
Insulin/gluc: Give 10 U insulin & 25 g dextrose (1 amp of D50). Hold D50 if bld gluc >250 mg/dL
Albuterol: 10–20 mg of 5 mg/mL nebulized solution
Sodium bicarbonate: Use only in pts w/ sev metabolic acidosis
Dialysis (hemodialysis faster at removing K+ than peritoneal dialysis)
Digitalis tox: Magnesium sulfate 2 g IV bolus. Do NOT use calcium (can potentiate digitalis tox)
Hypokalemia
• Definition: Serum potassium (K+) <3.5 mEq/L
• Clinical manifestations:
Muscle weakness
Nonspecific ECG changes: Prolonged QT interval, flattened inv T waves, U wave (Amp >1 mm)
Digitalis-induced arrhythmia
• Rx:
Treat causes of transcellular K+ shifts
Replace K+: KCl soln w/ 10, 20, 30, or 40 mEq K+. Infuse 20 mEq in 100 mL NS over 1 h
Replace serum magnesium
Hypercalcemia
• Definition: Total serum calcium >11 mg/dL, ionized calcium >3 mmol/L
• Clinical manifestations (seen when ionized calcium >3 mmol/L):
GI: Constip, N/V, ileus, pancreatitis
Renal: Polyuria, nephrocalcinosis
Neuro: Altered mental status, coma
Cardiovascular: HoTN, hypovolemia, decreased QT interval, AV block
• Rx & meds:
Correct hypovolemia: IV hydration w/ isotonic saline
Furosemide: 40–80 mg IV q2h to maintain urine output of 100 mL/h
Calcitonin: To ↓ bone resorption. 4 U/kg q12h SC or IM. Will ↓ serum calcium by 0.5 mmol/L
Hydrocortisone: 200 mg IV daily (divided 2–3 doses). Use w/ calcitonin.
Bisphosphonates: Max resp seen in 4–10 d
Zoledronate 4 mg IV, infuse over 15 min
Pamidronate 90 mg IV, infuse over 2 h
Hypernatremia
• Definition: Serum sodium (Na+) >145 mEq/L
• Clinical manifestations:
Altered mental status
Rhabdo
Absence of thirst vs. intense thirst
Polyuria
Diarrhea
• Diagnostic w/u/studies:
Document fluid intake & urine output
Serum osmolality, urine osmolality, urine electrolytes
• Rx & meds: (NEJM 2000;342:1493)
Stop any continuing causes of HyperNa
Correct serum sodium: Give hypotonic fluid PO or parenterally
Calculate water deficit & daily water loss
Total body water = total body weight × 0.5 in women
Free water deficit = [(serum Na – 140)/140] × TBW
Free water clearance = (V[1 – (UNa + UK)])/PNa
V = urine vol; UNa = urine [Na+]; UK = urine [K+]; PNa = plasma [Na+]
Insensible losses: 10 mL/kg/d
Replace daily water loss, correct water deficit
Chronic HyperNa: ↓ serum Na+ by 10 mmol/d
Avoid correcting too quickly to prevent cerebral edema
Acute HyperNa: ↓ serum Na+ by 1 mmol/L/h
Fluids: Give hypotonic fluids only (0.2% NaCl, 0.45% NaCl)
The more hypotonic the fluid, the lower the rate of infusion
Calculate change in serum Na+ w/ 1 L infusion:
[(infusion Na + infusion K) – serum Na+]/(total body water + 1)
Avoid dextrose solutions (hyperglycemia → osmotic diuresis → worsening HyperNa)
Avoid 0.9% NaCl
< div class='tao-gold-member'>



