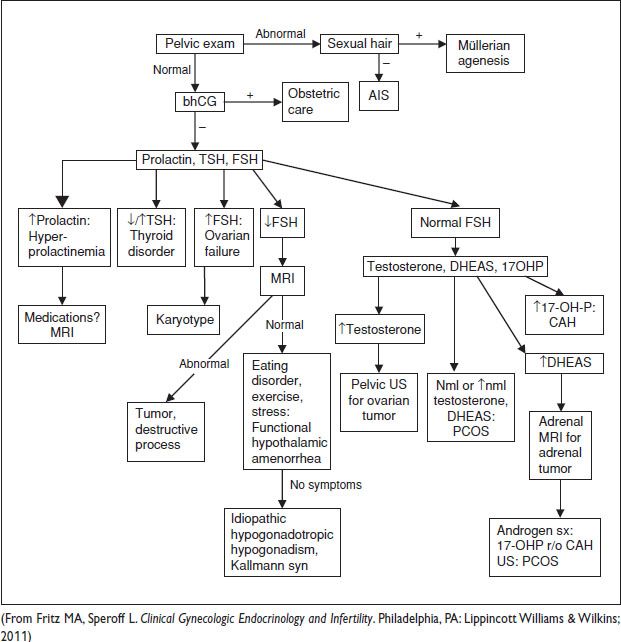
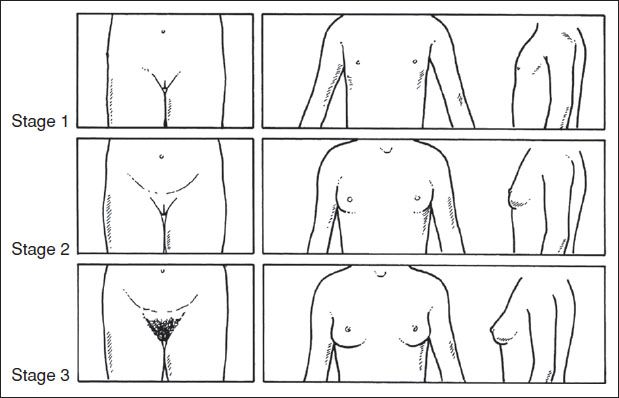
Figure 6.1 Tanner staging, female developmental stages
PRECOCIOUS PUBERTY
Definition (N Engl J Med 2008;358:2366)
• Dev of breast or pubic hair >2.5 SD below mean age. Traditional definition <8 yo. Trend of decreasing age of puberty → now <7 yo in C girls, <6 y in AA girls (Pediatrics 1997;99:505; Pediatrics 1999;104:936).
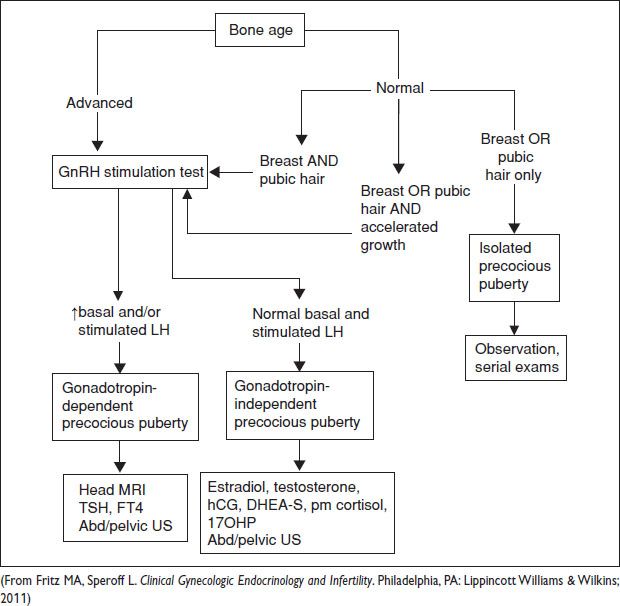
Initial Workup
• Hx: Onset, family members’ ages of puberty, h/o neurologic dz or trauma, exposure to sex steroids, headache, sz, abdominal pain
• PE: Height, weight, growth chart, Tanner staging, fundoscopic exam (papilledema in ↑ intracranial pres), visual field eval (sellar mass lesion), skin exam.
• Bone age eval: Plain film X-ray of left hand & wrist
• Lab eval: Basal LH, LH following GnRH stimulation, FSH, estradiol
LH <0.1 IU/L = premature thelarche or nml
LH >0.3 IU/L = true precocious puberty
LH >5 mIU/L = central (gonadotropin-dependent) precocious puberty
Treatment Goals
• Postpone dev until nml pubertal age, maximize adult height, reduce risk of psychosocial problems a/w early sexual maturation
Gonadotropin-dependent (Central) Precocious Puberty (GDPP)
• Early maturation of HPO axis → breast & pubic hair dev, w/ usually nml sequence of pubertal events at nml pace, & isosexual (appropriate for gender)
• Etiology: Idiopathic – 90%; dx of exclusion. CNS lesions – tumors, irradiation, hydrocephalus, cysts, trauma, inflamm dz, midline developmental defects. Sev hypothyroidism (rare).
• Dx: Accelerated linear growth for age (>75% of height at dx), advanced bone age, pubertal levels of FSH, LH, estradiol, & ↑ w/ GnRH stimulation test. MRI in all pts to evaluate for CNS lesion. TFTs if clinical concern for hypothyroidism. Evaluate ↓ growth hormone if h/o cranial irradiation. Abdominopelvic US – repeated exposure to sex steroids from periph sources can induce secondary premature maturation of HPO axis.
• Rx: Treat intracranial lesions or hypothyroidism if present. Idiopathic GDPP, treat if:
sexual maturation progresses to next stage w/i 3–6 mo,
onset puberty <6 yo,
growth velocity >6 cm/y,
Bone age advanced by 1 y or more, or
predicted adult height below target range or decreasing on serial determinations.
Long-acting GnRH agonist → prepubertal hormone level, prevents pubertal dev, growth acceleration, & bone advancement (N Engl J Med 1981;305:1546). Treat until epiphyses fused or pubertal & chrono ages are appropriately matched.
Gonadotropin-independent (Peripheral) Precocious Puberty
• Due to excess exposure of sex steroid hormones from gonads, adrenals, or environment. May be contrasexual or isosexual. Pubertal sequence progression may be altered.
• Etiology: Functional ovarian follicular cysts – most common cause, w/ transient breast dev & vaginal bleeding, 1+ unilateral or bilateral ovarian cysts >15 mm, bone age nml. Ovarian tumors (rare) – granulosa cell tumor → isosexual, Leydig cell/gonadoblastoma → contrasexual. Adrenal – androgen-secreting tumors, CAH. McCune–Albright syndrome (rare) – triad of periph precocious puberty, café-au-lait spots, fibrous bone dysplasia → recurrent formation of follicular cysts & cyclic vaginal bleeding.
• Dx: Low or nml FSH & LH levels, do not ↑ w/ GnRH stimulation. Labs: Testosterone, estradiol, FSH, afternoon cortisol (screen Cushing syn), DHEA, DHEAS, 17-OHP (screen CAH). Abdominopelvic US for ovarian cyst/tumor.
• Rxs: Surgical removal (tumor); tamoxifen for vaginal bleeding, bisphosphonate for bone dysplasia; aromatase inhibs lack long-term effectiveness; exogenous estrogens as cream, ointment, spray (contrasexual); remove exogenous source; for functional cysts → observation, usually self-limited, surgical removal if persistent or torsion; GnRH agonist ineffective for gonadotropin independent.
Isolated Precocious Puberty
• Isolated premature thelarche or adrenarche. Usually benign nml variants. If bone age nml, precocious puberty unlikely.
• Expectant mgmt w/ re-evaluation at 6 mo. ∼20% progress to gonadotropin-dependent precocious puberty. Requires regular exams.
• Isolated premature thelarche: Unilateral or bilateral, <8 y, absence of other secondary sexual characteristics, nml linear growth, nml bone age. Estradiol level usually prepubertal – girls typically <3 yo, nonobese. Unk cause.
• Isolated premature adrenarche: Isolated pubic &/or axillary hair <8 y. Dx: DHEA-S appropriate for pubic hair stage. Girls typically overweight. 17-OHP & testosterone appropriate for age. Bone age & growth rate ↑ but w/i nml limits. Risk factor for PCOS. Further w/u: ACTH stimulation to r/o CAH when bone age advanced, predicted adult height abnormally low, or serum testosterone & DHEA-S elevated – may be only manifestation of mild CAH. Rx: Observation, regular exams to detect other signs of precocious sexual dev.
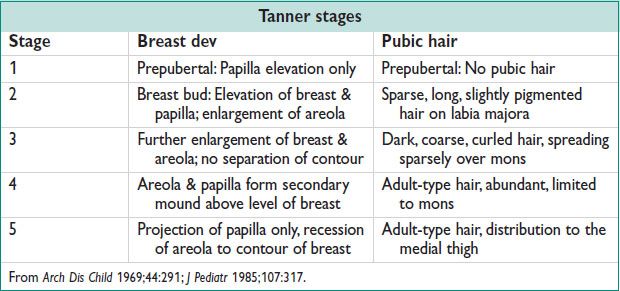
Figure 6.2 Approach to precocious puberty
DELAYED PUBERTY
Definition (N Engl J Med 2012;366:443; Pediatr Clin North Am 2011;58:1181)
• Absence of secondary sexual characteristics by age 13 (≥2 SD from mean age), or absence of menses by age 15.
Etiology (J Clin Endocrinol Metab 2002;87:1613)
• 30% const del, 26% hypergonadotropic hypogonadism, 20% permanent hypogonadotropic hypogonadism, 19% transient (functional) hypogonadotropic hypogonadism, 5% other causes.
Clinical Manifestations
• Hx: Anorexia, bulimia, excessive exercise, chronic dzs (eg, celiac dz, Crohn dz), radiation, chemo, meds, nutritional status, psychosocial functioning
• Sx: Neurologic sx, inability to smell, weight gain or loss, chronic dz
• FHx: Relatives w/ delayed puberty, heights of relatives, age of menarche & fertility status of female relatives, relatives w/ genetic abnormalities (CAH, adenocarcinoma in situ (AIS), gonadal dysgenesis), relatives w/ autoimmune dz
Physical Exam
• Height & weight measurements, growth chart, Tanner staging, examine for stigmata of Turner syn, midline facial defects, scoliosis, thyromegaly.
• Arm span greater than height >5 cm sugg delayed epiphyseal closure
• Neurologic exam: Optic fundi, cranial nerves, visual fields, sense of smell
• Pelvic exam: Clitoral enlargement, hymenal ring patency, degree of vaginal rugation, presence or absence of mucus (indicates degree of estrogen effect)
Workup
• Hx, physical exam, bone age, labs (LH, FSH)
Elevated FSH/LH = hypergonadotropic hypogonadism
Low FSH/LH = hypogonadotropic hypogonadism
• Further w/u if LH, FSH nml:
PRL – screen for hyperprolactinemia
TSH, FT4 – screen for thyroid dzs
MRI – when si/sx CNS lesion present or if indicated by other eval (hyperprolactinemia, Kallmann syn); otherwise may defer until age 15
CBC, ESR, LFTs – screen chronic dzs (IBD, liver dz, anorexia)
Pelvic US – determine presence/absence uterus if undetermined by physical exam
• Unusually no apparent alternate cause on initial eval – const del likely dx; no test can reliably differentiate const del from hypogonadotropic hypogonadism; therefore, observe, & diagnose isolated hypogonadotropic hypogonadism if endogenous puberty has not begun by age 18; eventual nml progression of puberty confirms const del.
Treatment Goals
• Induce appearance of secondary sexual characteristics or acceleration of growth to mitigate pubertal delay & short stature, & promote nml bone mass
• Predict adult height w/ Bayley-Pinneau tables, although overestimate adult height in const del.
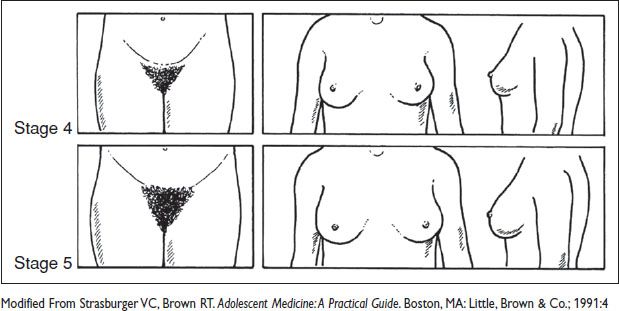
Figure 6.3 Approach to delayed puberty
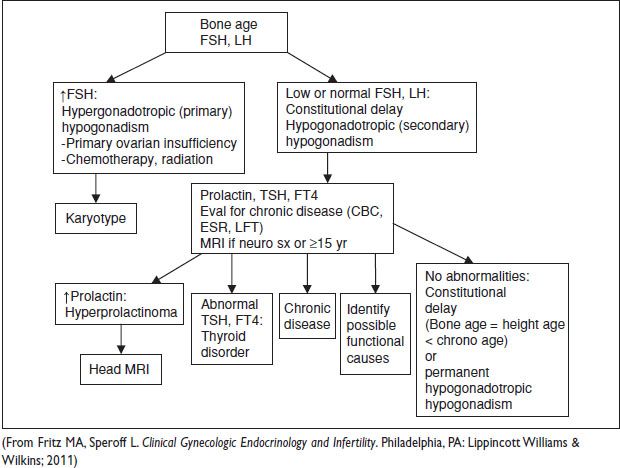
Hypergonadotropic (Primary) Hypogonadism
• Dx: Elevated LH & FSH due to lack of negative feedback from gonads. Additional w/u: Karyotype, autoimmune dz eval.
• Etiology: Primary ovarian insufficiency (idiopathic, resistant ovary syn, autoimmune oophoritis, 17a-hydroxylase deficiency, galactosemia, aromatase deficiency), Gonadal dysgenesis (45,X; 46,XX; 46,XY), radiation, chemo. Special cases:
Turner syn: 45,X (Semin Reprod Med 2011;29:342) – phenotype: Female, short stature, ptosis, low-set ears, micrognathia, short “webbed” neck, broad shield-like chest, hypoplastic areolae, short 4th &/or 5th metacarpals, renal abnormalities (eg, horseshoe kidney), cardiovascular abnormalities (eg, coarct of the aorta). Risk of aortic dissection & rupture (1.5%). “Streak” gonads consist of fibrous tissue w/o germ cells. External female genitalia, uterus, fallopian tubes develop normally until puberty when estrogen-induced maturation fails to occur. Menstruation & Preg may occur in mosaic karyotype (45,X/46,XX). Rx: Growth hormone prior to estrogen initiation.
Swyer syn: 46,XY complete gonadal dysgenesis. Phenotype: Female, w/ vagina, cervix, uterus, fallopian tubes, & external genitalia. Rx: Requires early gonadectomy due to risk of gonadal tumors.
Primary ovarian insufficiency: See Chap. 8.
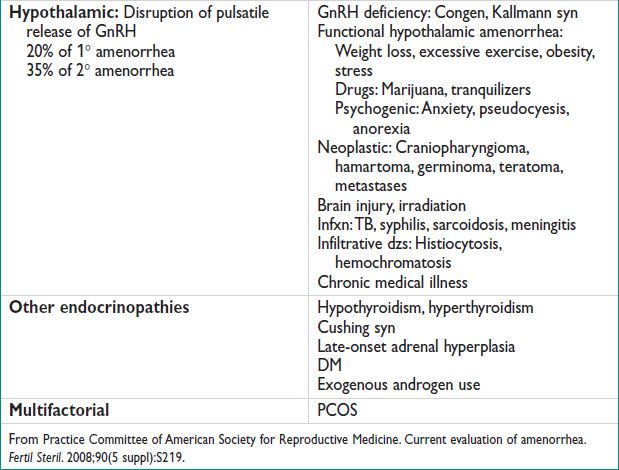
Permanent Hypogonadotropic (Secondary) Hypogonadism
• Dx: Low to nml LH & FSH due to hypothalamic or pituitary disorders.
• Etiology: GnRH deficiency, CAH, CNS tumors, combined pituitary hormone deficiency, chemo, radiation
Kallmann syn: Anosmia or hyposmia; 1/50000 females
• Further w/u: MRI
• Rx: Initial low-dose estrogen titrated to mimic nml puberty to initiate sexual maturation
After 6–9 mo, cyclic progesterone to induce endometrial shedding
Transition to combination OCP when breast dev optimized for hormonal replacement
If fertility desired, pulsatile GnRH or injectable gonadotropin
Transient (Functional) Hypogonadotropic Hypogonadism
• Dx: Low LH & FSH due to delayed maturation of HPO axis due to underlying condition
• Etiology: Systemic illness (IBD, celiac dz, anorexia nervosa or bulimia, hypothyroidism, hyperprolactinemia, DM, Cushing dz), CNS disorders (tumors [eg, craniopharyngioma, prolactinoma], infxn, trauma), adrenal (Cushing syn, Addison dz), psychosocial (excessive exercise, stress, depression), drugs (marijuana).
• Rx: Treat underlying cause (treat dz or modify behavior)
• Const Del:
Dx: Low LH & FSH, HA = bone age < chrono age. Adrenarche & gonadarche often later than avg; isolated hypogonadotropic hypogonadism has adrenarche at nml age.
Rx: Expectant observation. If puberty has started (clinically or biochemically) & stature not a major concern, reassurance w/ adult height prediction.
Hormone rx is controversial (goal of preventing developmental psychosocial stress). Use low-dose estrogen until puberty progresses, then stop. Progesterone not needed as similar long period of unopposed estrogen in early puberty. Growth hormone, anabolic steroids, aromatase inhibs not recommended.
AMENORRHEA
Definitions (Pediatrics 2006;118:2245; Obstet Gynecol Clin North Am 2003;30:287)
• Primary amenorrhea: Absence of menstruation by age 13–14 in absence of growth or sexual dev, or age 15–16 in presence of nml growth & sexual dev
• Secondary amenorrhea: Absence of menses for ≥3 consecutive menstrual cycles in women w/ previously nml menses
Epidemiology
• Primary amenorrhea 1–2% prevalence in US. Amenorrhea not caused by Preg ≤5% prevalence during menstrual lives. Most common causes of primary amenorrhea: Ovarian failure (48.5%), Müllerian agenesis (16.2%), gonadotropin deficiency (8.3%), constitutional delay (6%) (Am J Obstet Gynecol 1981;140:372).
History
• Hx: Stress, change in weight, diet, exercise, sugg functional hypothalamic etiology
New meds – evaluate for hyperprolactinemia due to meds
New illnesses – sugg chronic illness etiology
Acne, hirsutism, deepening of voice – sugg hyperandrogenism: PCOS or adrenal etiology
Headache, visual field defects, fatigue, polyuria, polydipsia – sugg CNS lesion
Hot flashes, vaginal dryness, poor sleep, decreased libido – sugg primary ovarian insufficiency
Galactorrhea – sugg hyperprolactinemia
H/o postpartum hemorrhage, D&C, endometritis – sugg Asherman or Sheehan syn
Physical Exam
• Height, weight (BMI <18.5 at risk for functional hypothalamic amenorrhea; BMI >30 in ∼50% pt w/ PCOS.
• Tanner staging if primary amenorrhea. Assess estrogen status: Adequate if breasts present, moist & rugated vaginal mucosa, abundant cervical mucus.
• Assess for presence of uterus, cervix, or signs of obstructed tract.
• Assess for signs of excessive testosterone: Hirsutism, acne, acanthosis nigricans
• Evaluate for galactorrhea
• Parotid gland swelling &/or erosion of dental enamel sugg bulimia nervosa
• Evaluate for stigmata of Turner syn.
Initial Workup
• History & physical exam. Lab: Urine hCG, TSH, FSH, PRL (↑ by stress, sleep, intercourse, meals, nipple stimulation). If signs of hyperandrogenism: Testosterone, ± 17-OHP (CAH), DHEA-S (adrenal etiology).
• Progesterone challenge test: Determine if adequate estrogen present, competent endometrium, patent outflow. Medroxyprogesterone acetate 10 mg PO daily for 7–10 d.
• Withdrawal bleed expected w/i 2–7 d of stopping progesterone:
+ bleed: Nml estrogen production & ovarian fxn
– bleed: Hypoestrogenic or anatomic outflow tract obst
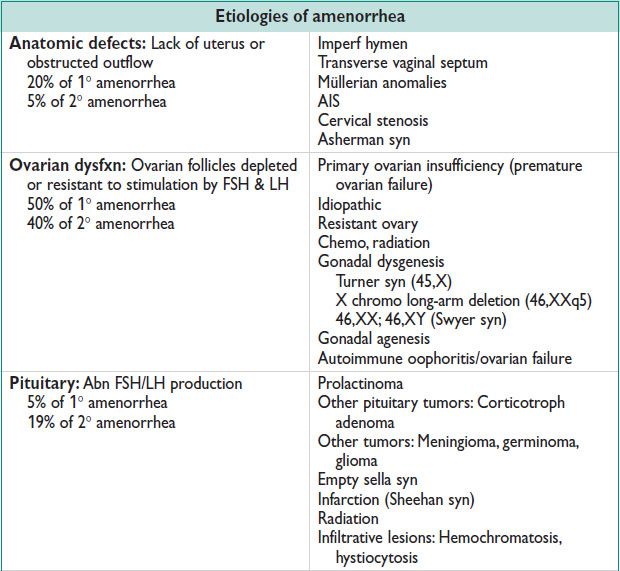
Congenital Anatomic Lesions
• Menses cannot occur w/o an intact uterus, endometrium, cervix, vaginal conduit. Clinical manifestations: Cyclic pelvic &/or lower abdominal pain from accum & subseq dilation of vaginal vault &/or uterus by menstrual bld.
• Imperf hymen: Bulging membrane just inside the vagina, often purple-red discoloration.
• Transverse vaginal septum: Occurs at any level btw hymenal ring & cervix; absence of bulging hymen as septum much thicker.
• Vaginal agenesis: See Chap. 8.
• Rx: Surgical correction
Asherman Syndrome (Semin Reprod Med 2011;29:83)
• Acq scarring of the endometrial lining, usually secondary to postpartum hemorrhage or endometrial infxn followed by dilation & aggressive curettage. Prevents nml buildup & shedding of endometrial cells → very light or absent menses.
• HSG shows uterine filling defects. No withdrawal bleed following estrogen & progesterone. Hysteroscopic eval demonstrates uterine synechiae.
• Rx: Surgical lysis of adhesions by hysteroscopy. Estrogen postoperatively to help promote endometrial regeneration.
Primary Ovarian Insufficiency (Premature Ovarian Failure)
See Chap. 8.
Hyperprolactinemia (Curr Opin Obstet Gynecol 2004;16:331; J Reprod Med 1999;44:1075)
• Etiology: Hypothyroidism, PRL-secreting pituitary adenomas (20% secondary amenorrhea), pituitary or hypothalamic tumors, meds (amphetamines, benzodiazepines, metoclopramide, methyldopa, opiates, phenothiazines, reserpine, tricyclic antidepressants, SSRIs). Occurs due to dopamine receptor antagonism.
• Clinical manifestations: ± galactorrhea.
• Dx: Elevated serum PRL; r/o hyperthyroidism. Further w/u: MRI to evaluate for pituitary tumor if persistent ↑ PRL or >100 ng/mL
• Rx: Dopamine agonist (bromocriptine or cabergoline) or transsphenoidal resxn of CNS lesion.
Sheehan Syndrome
• Acute infarction & ischemic necrosis of pituitary gland from postpartum hemorrhage & hypovolemic HoTN. More common in low resource settings.
• Clinical manifestations: Failed postpartum lactation, fatigue, weight loss, loss of sexual hair
• Dx: Hx, growth hormone, LH, FSH, PRL, ACTH, TSH deficiencies.
Functional Hypothalamic Amenorrhea (N Engl J Med 2010;363:365)
• Abn GnRH pulses → decreased gonadotropin pulsations → low/nml serum LH concentrations → absent LH surge → absence of follicular dev, anovulation, low estradiol.
• Etiology: Stress, weight change, decreased nutrition, excessive exercise, anorexia nervosa or bulimia, chronic dz (DM, ESRD, malig, AIDS, IBD), isolated gonadotropin deficiency (congen, Kallmann syn), Sheehan syn.
• W/u: MRI for CNS/hypothalamic/pituitary dz.
• Rx: Behavior modification if indicated, treat chronic dz, hormonal therapy to prevent bone loss, ovulation induction w/ clomiphene citrate, gonadotropin injection, pulsatile GnRH.
Polycystic Ovarian Syndrome (PCOS)
See Chap. 8.
Figure 6.4 Approach to amenorrhea