14.1 Acute upper respiratory infections
Because of their frequency, upper respiratory tract infections (URTIs) are a major burden for young children and their parents. Although the common cold is the most common ailment in humans, it is particularly frequent in preschool-aged children, who average six to eight episodes per year. The timing and frequency of these infections depends on the level of exposure, occurring earlier and more often in those with older siblings, and those who attend daycare (Fig. 14.1.1). The vast majority of URTIs are viral in origin, mild, and of short duration (5–7 days), and usually described as a ‘common cold’. Numerous different viruses are responsible, and the age of the child and the specific respiratory virus are the major predictors of the symptoms, severity and extent of respiratory tract involvement (Tables 14.1.1, 14.1.2).
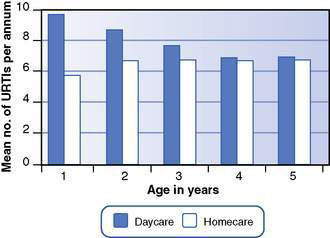
Fig. 14.1.1 Number of respiratory tract infections per year in infants and preschoolers (daycare versus homecare).
(From data in Isaacs D, Moxon ER 1996.)
Table 14.1.1 Age of child and type of respiratory tract infection
| Age | Type of infection |
|---|---|
| Newborn | Risk of acute, generalized systemic illness with respiratory syncytial virus (looks ‘septic’) |
| Infant | High risk of lower respiratory tract involvement with respiratory viruses (particularly acute viral bronchiolitis from respiratory syncytial virus) |
| Toddler/preschooler | Very frequent viral respiratory tract infections, mostly confined to upper respiratory tract |
| High risk of viral laryngotracheobronchitis (‘croup’) from parainfluenza viruses | |
| School age (5–15 years) | Lower rates of viral respiratory tract infection |
| Suspect: |
Table 14.1.2 Incubation period of viral respiratory infections
| Virus | Median incubation period (95% confidence interval) |
|---|---|
| Influenza A | 0.6 (0.5 to 0.6) days |
| Rhinovirus | 1.9 (1.4 to 2.4) days |
| Parainfluenza | 2.6 (2.6 to 3.1) days |
| Adenovirus | 3.2 (2.8 to 3.7) days |
| Respiratory syncytial virus | 4.4 (3.9 to 4.9) days |
| Influenza B | 12.5 (11.8 to 13.3) days |
Respiratory complications
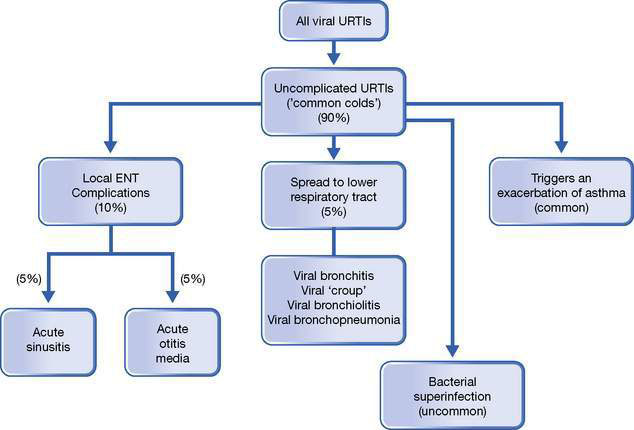
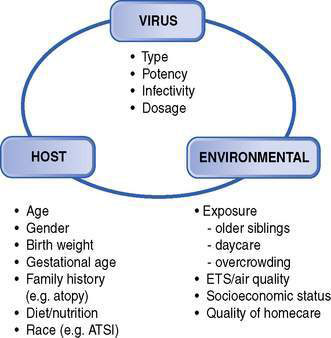
The importance of these recurring infections of early childhood should not be underestimated. A significant percentage of children will suffer from local complications of viral URTIs, especially acute otitis media and acute sinusitis (Fig. 14.1.2). Moreover, progression of the infection into the lower respiratory tract is a risk, particularly in the very young. This is especially likely with the more potent respiratory viruses, such as respiratory syncytial virus (RSV – the usual cause of acute viral bronchiolitis), parainfluenza (the usual cause of viral ‘croup’), influenza virus (A and B) and the recently recognized human metapneumovirus (HMP – a close relative of RSV). Some children are particularly vulnerable to these lower respiratory tract complications, suggesting additional important host and environmental factors (Fig. 14.1.3).
Incubation period of viral respiratory infections
Knowledge of the incubation period of these respiratory viruses is useful when considering the likely timing of infection, the source and quarantine decisions. A systematic review of over 400 publications described the median incubation period (and 95% confidence intervals) for the respiratory viruses of public health importance; these are listed in Table 14.1.2. Most have a short incubation period, with symptoms generally developing within 2–3 days of exposure.
Identifiable URTI syndromes
Common cold (uncomplicated viral URTI or ‘head cold’)
This is defined as an acute illness where the major symptoms are:
The symptoms are mild, fever is often minimal or absent, and all symptoms resolve between 5 and 7 days. The usual pathogen responsible for an uncomplicated viral URTI is rhinovirus, which has over 100 types. However, there are many other respiratory viruses that can produce this syndrome (see Table 14.1.2). These viruses are highly infectious and spread via both droplets (particularly by sneezing) and nasal secretions on hands and fomites (clothing, handkerchiefs, toys, cot sides). Viral shedding is maximal in the 7 days after inoculation and most have a short incubation period (2–3 days). Therefore, close proximity such as household contacts with older school-aged siblings, daycare attendance, overcrowding, lower socioeconomic status and poor personal hygiene are all associated with higher rates of URTI (see Fig. 14.1.3).
Local ENT complications of the common cold include otitis media and acute rhinosinusitis (see Fig. 14.1.2), and a small proportion progress to involve the lower respiratory tract.