49 Acute Rheumatic Fever and Rheumatic Heart Disease
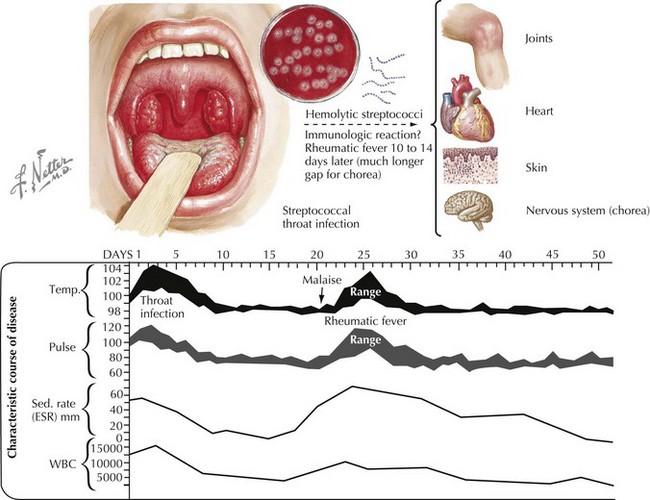
Acute rheumatic fever (ARF) is postulated to be caused by a delayed systemic autoimmune reaction to group A β-hemolytic streptococcal (GAS) pharyngitis. It is a self-limited disease that may involve the heart, skin, brain, joints, and serosal surfaces (Figure 49-1). It is a disease of clinical interest primarily because of its propensity to create heart disease. Rheumatic carditis and valvulitis may be self-limited or may lead to progressive valve deformity.
Etiology And Pathogenesis
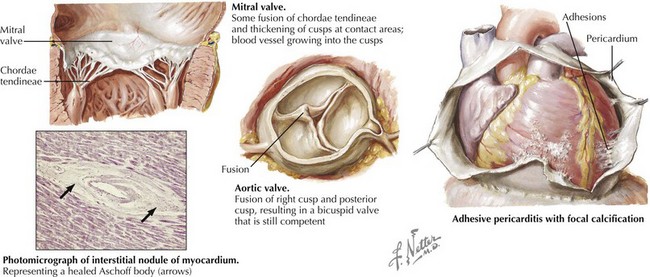
The virulence of GAS is related to the bacterial M protein, which structurally resembles human myosin. It is presumed that GAS adheres to the pharyngeal mucosa of the patient and activates antigens and superantigens, which triggers an immune response. In genetically susceptible individuals, antibodies against myosin are produced, which can lead to carditis. Repeated untreated infections with GAS may reactivate antibody production and lead to an autoimmune response that lasts several weeks and eventually damages heart valves (Figure 49-2).
Clinical Presentation
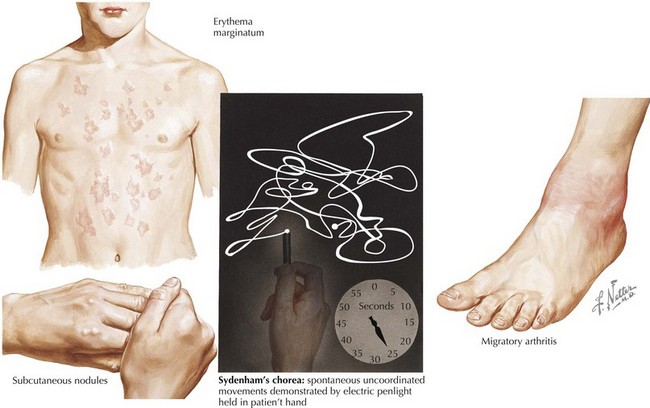
More than 60 years ago, T. Duckett Jones published guidelines for diagnosis of ARF that have been slightly revised by the World Health Organization (Box 49-1 and Figure 49-3). To make a primary diagnosis of ARF, two major or one major and two minor criteria plus evidence of a preceding GAS infection are needed. The exception is rheumatic chorea. Sydenham’s chorea (St. Vitus dance) in isolation is considered diagnostic, and no other criteria or evidence of GAS infection are required to make the diagnosis.
Box 49-1 2002 to 2003 World Health Organization Revision of Jones Criteria for the Diagnosis of Rheumatic Fever
Major Criteria
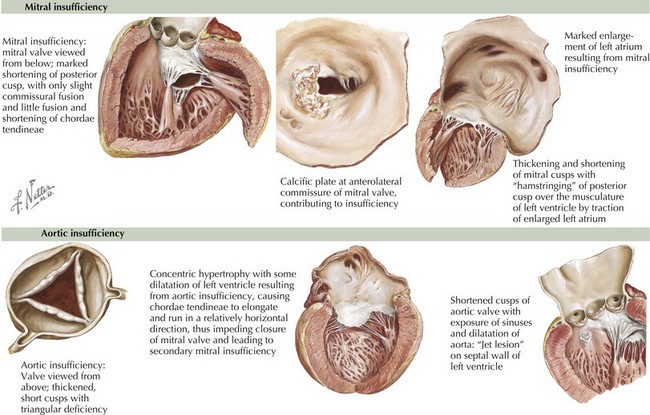
A history of ARF is obtained in only 60% of patients with RHD. Whereas chronic mitral regurgitation is the most common form of RHD in children and young adults (Figure 49-4), mitral stenosis is more common in older adults. Aortic regurgitation, although less common than mitral regurgitation with ARF, is more likely to persist (see Figure 49-4). Patients with mitral or aortic valve disease may present with an isolated heart murmur or palpitations caused by atrial arrhythmias. They can present with fatigue, decreased exercise tolerance, dyspnea on exertion, orthopnea, and paroxysmal nocturnal dyspnea, which can represent low cardiac output or pulmonary hypertension. However, the onset of symptoms can often be so insidious that patients adapt and are unaware of their significant functional limitations.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree