Chapter 66 Acute Care of the Victim of Multiple Trauma
Epidemiology
Injury is a leading cause of death and disability in children throughout the world (Chapter 5.1). According to the World Health Organization report on child injury prevention, unintentional injuries are one of the leading causes of death in children younger than 20 yr and the leading cause of death in children between 10 and 20 yr in the world. Road traffic accidents, drowning, fire-related events, and falls rank among the top causes of death and disability in children. In Asia, injury accounts for more than 50% of deaths in children <18 yr, with drowning accounting for approximately half. In the USA, more than 12,000 children die each year secondary to unintentional injury, with motor vehicle related injuries being the leading cause.
Regionalization and Trauma Teams
Mortality and morbidity rates have decreased in geographic regions with comprehensive, coordinated trauma systems. Treatment at designated trauma centers is associated with decreased mortality. At the scene of injury, paramedics should administer necessary advanced life support and perform triage (Fig. 66-1; Tables 66-1 and 66-2). It is usually preferable to bypass local hospitals and rapidly transport a seriously injured child directly to a pediatric trauma center (or a trauma center with pediatric commitment). Children have lower mortality rates after severe blunt trauma when they are treated in designated pediatric trauma centers or in hospitals with pediatric intensive care units.
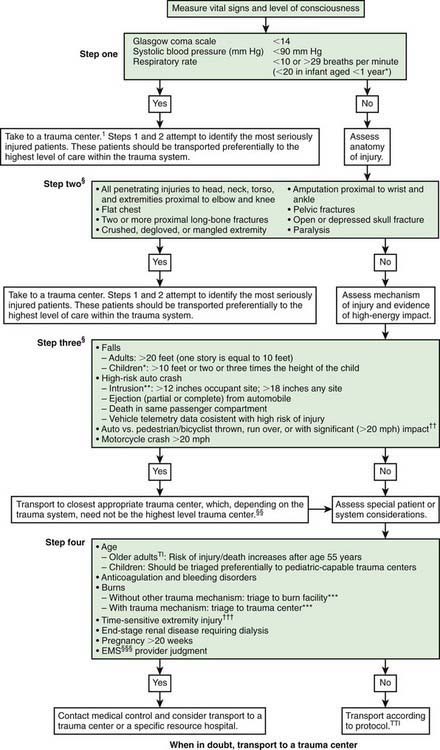
Figure 66-1 Field triage decision scheme—United States, 2006.
§Any injury noted in Steps 2 and 3 triggers a “yes” response.
†††Injuries such as an open fracture or fracture with neurovascular compromise.
§§§Emergency medical services.
Table 66-1 CHANGES IN FIELD TRIAGE DECISION SCHEME CRITERIA FROM 1999 TO 2006 VERSION*
STEP ONE: PHYSIOLOGIC CRITERIA
STEP TWO: ANATOMIC CRITERIA
STEP THREE: MECHANISM-OF-INJURY CRITERIA
STEP FOUR: SPECIAL CONSIDERATIONS
* Scheme is shown in Fig. 66-1.
Modified from Sasser SM, Hunt RC, Sullivent EE, et al: Guidelines for field triage of injured patients: recommendations of the National Expert Panel on Field Triage, MMWR Recomm Rep 58(RR-1):1–35, 2009. http://www.cdc.gov/mmwr/PDF/rr/rr5801.pdf.
Table 66-2 CHILDREN REQUIRING PEDIATRIC TRAUMA CENTER CARE
Modified from Krug SE: The acutely ill or injured child. In Behrman RE, Kliegman RM, editors: Nelson essentials of pediatrics, ed 4, Philadelphia, 2002, WB Saunders, p 96.
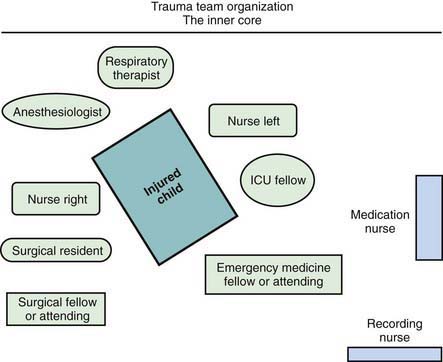
When the receiving ED is notified before the child’s arrival, the trauma team should also be mobilized in advance. Each member has defined tasks. A senior surgeon (surgical coordinator) or, sometimes initially, an emergency physician leads the team. Team compositions vary somewhat from hospital to hospital; the model used at Children’s National Medical Center (Washington, DC) is shown in Figure 66-2. Consultants, especially neurosurgeons and orthopedic surgeons, must be promptly available; the operating room staff should be alerted.
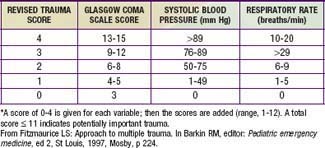
Physiologic status, anatomic locations, and/or mechanism of injury are used for field triage as well as to determine whether to activate the trauma team (see Table 66-2). More importance should be placed on physiologic compromise and less on mechanism of injury. Scoring scales such as the Abbreviated Injury Scale (AIS), Injury Severity Score (ISS), Pediatric Trauma Score, and Revised Trauma Score (Table 66-3) use these parameters to predict patient outcome. The AIS and ISS are used together. First, the AIS is used to numerically score injuries—as 1 minor, 2 moderate, 3 serious, 4 severe, 5 critical, or 6 probably lethal—in each of 6 ISS body regions: head/neck, face, thorax, abdomen, extremity, and external. The ISS is the sum of the squares of the highest 3 AIS region scores.
Primary Survey
Breathing
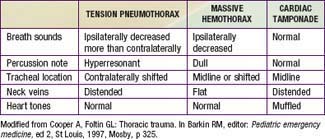
Although less common than a pulmonary contusion, tension pneumothorax and massive hemothorax are immediately life-threatening (Tables 66-4 and 66-5). Tension pneumothorax occurs when air accumulates under pressure in the pleural space. The adjacent lung is compacted, the mediastinum is pushed toward the opposite hemithorax, and the heart, great vessels, and contralateral lung are compressed or kinked (Chapter 405). Both ventilation and cardiac output are impaired. Characteristic findings include cyanosis, tachypnea, retractions, asymmetric chest rise, contralateral tracheal deviation, diminished breath sounds on the ipsilateral (more than contralateral) side, and signs of shock. Needle thoracentesis, followed by thoracostomy tube insertion, is diagnostic and lifesaving. Hemothorax results from injury to the intercostal vessels, lungs, heart, or great vessels. When ventilation is adequate, fluid resuscitation should begin before evacuation, because a large amount of blood may drain through the chest tube, resulting in shock.
Table 66-4 LIFE-THREATENING CHEST INJURIES
TENSION PNEUMOTHORAX
OPEN PNEUMOTHORAX (SUCKING CHEST WOUND)
Effect on ventilation depends on size
MAJOR FLAIL CHEST
MASSIVE HEMOTHORAX
CARDIAC TAMPONADE
Beck Triad:
Modified from Krug SE: The acutely ill or injured child. In Behrman RE, Kliegman RM, editors: Nelson essentials of pediatrics, ed 4, Philadelphia, 2002, WB Saunders, p 97.
Circulation
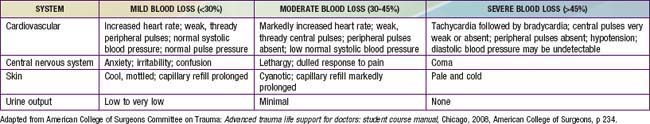
The most common type of shock in trauma is hypovolemic shock due to hemorrhage. Signs of shock include tachycardia; weak pulse; delayed capillary refill; cool, mottled, pale skin; and altered mental status (Chapter 64). Early in shock, blood pressure remains normal because of compensatory increases in heart rate and peripheral vascular resistance (Table 66-6). Some individuals can lose up to 30% of blood volume before blood pressure declines. It is important to note that 25% of blood volume equals 20 mL/kg, which is only 200 mL in a 10-kg child. Losses >40% of blood volume cause severe hypotension that, if prolonged, may become irreversible. Direct pressure should be applied to control external hemorrhage. Blind clamping of bleeding vessels, which risks damaging adjacent structures, is not advisable.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree