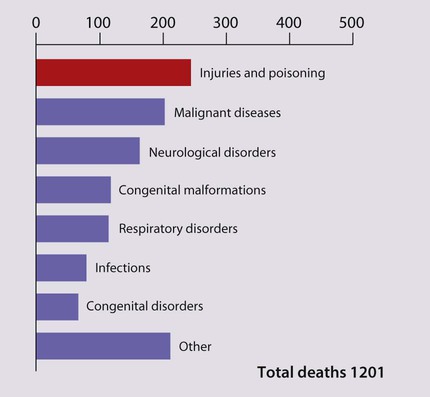
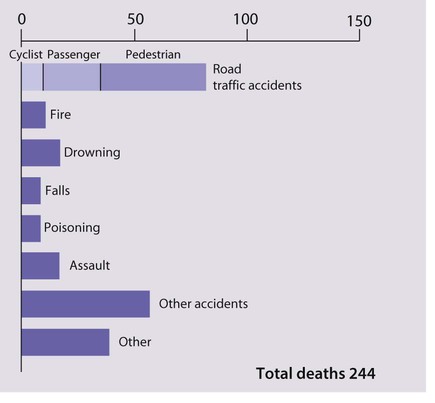
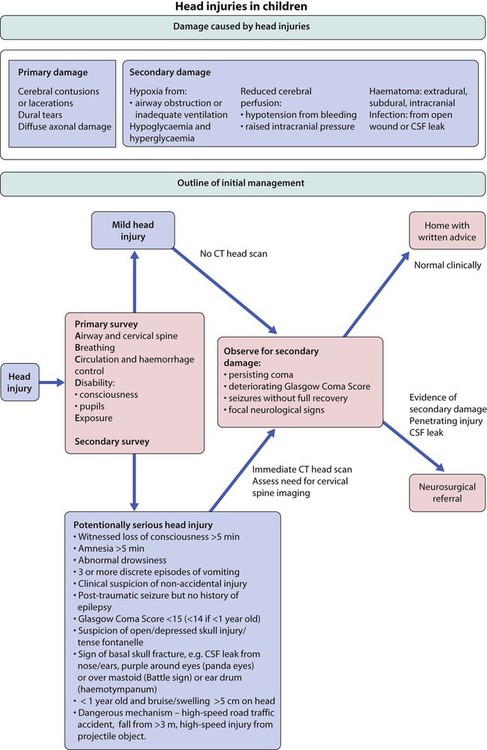
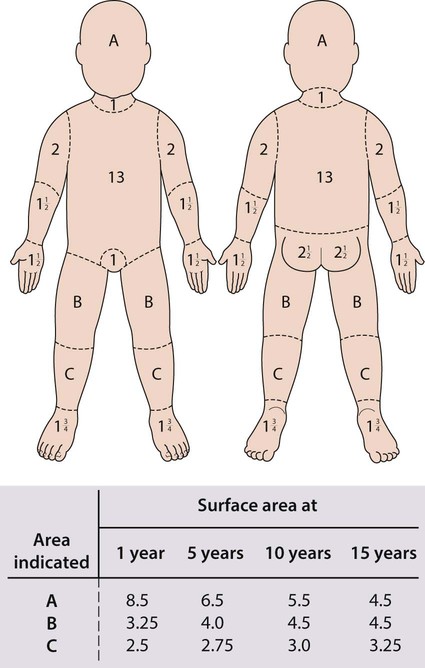
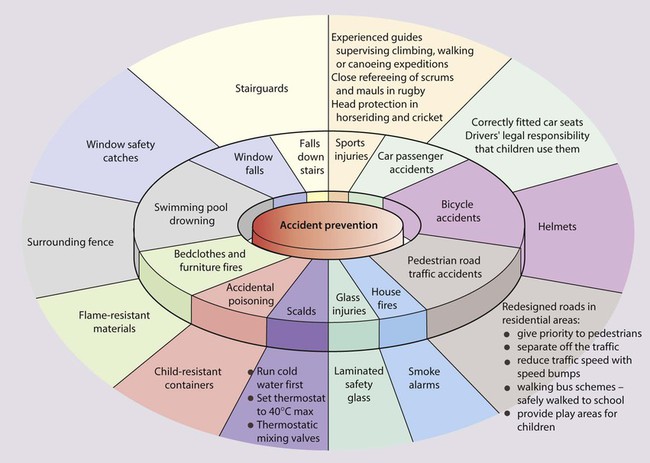
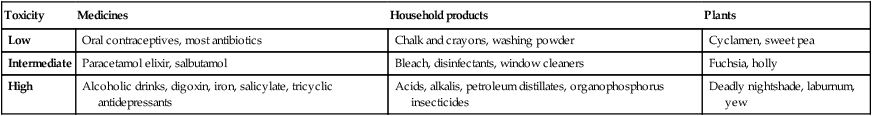
The risk of accidents, poisons and abuse is increased by: • Poor-quality, overcrowded homes • Lack of a safe environment for play • Poor parenting skills, which may be due to parental psychiatric illness, drug and alcohol abuse, violent temperament, poor education or lack of social support. Accidents (now often called ‘unintentional injuries’) are extremely common. In the UK, one in four children attend an A&E department each year; about half because of an accident. They are more common in boys. Most accidents cause only minor injury but can also be fatal. Injuries, mostly accidents, and poisoning are the major cause of death in children 1–14 years of age in the UK (Figs 7.1, 7.2). Accidents also cause significant disability and suffering, including post-traumatic stress disorder. Head injury with brain damage is the major cause of disability from accidents. Cosmetic damage following burns, scalds and other accidents may cause the child profound psychological harm. The prevention of childhood accidents is clearly important. Doctors and nurses who treat children and see the effects of accidents are particularly well placed to provide the community with advice on appropriate preventive measures (Fig. 7.3). In order to prevent accidents: • The relationship between an individual type of accident and the child’s developmental level must be considered • Specific solutions should be based on detailed epidemiology, e.g. child-resistant containers are the best method to limit children’s access to medicines Minor head injuries in childhood are common, and the vast majority of children recover without suffering any ill effects. However, about 1 in 800 of these children develop serious problems. The aim of the management of head injuries is to identify those children requiring treatment and to avoid secondary damage to the brain from hypoxia or poor cerebral perfusion (Fig. 7.4). Head injury may result in concussion, a reversible impairment of consciousness, a subdural or extradural haematoma or intracerebral contusion (see Ch. 27). Children may suffer internal injuries associated with severe trauma. These include: • Abdominal injuries, including a ruptured spleen, ruptured liver, kidney and bowel. There should be a high index of suspicion for these internal injuries if there has been abdominal trauma or if the clinical setting suggests significant inflicted, i.e. abusive, injury. The child needs close observation. Abdominal ultrasound (focused abdominal sonography in trauma – FAST scan) and X-rays, including CT scan, may be helpful. If there is any doubt, a laparotomy/laparoscopy is undertaken. Intra-abdominal injuries such as a contained splenic bleed are increasingly managed conservatively with close monitoring, but paediatric surgical support must be available immediately in case surgery is required. • Chest injuries, including pneumothorax and haemopericardium, may require emergency treatment. These children should be managed in a paediatric intensive care unit. The severity of the injury is assessed: • Is the airway, breathing and circulation satisfactory? • Was there any smoke inhalation? If this has occurred, there is a danger of subsequent respiratory complications and carbon monoxide poisoning. All affected children should be observed and managed in hospital, with a low threshold to protect the airway before secondary problems develop. • Depth of the burn. In superficial burns, the skin will be epithelialised from surviving cells. In partial thickness burns, there is some damage to the dermis with blistering, and the skin is pink or mottled; regeneration for superficial and partial thickness burns is from the margins of the wound and from the residual epithelial layer surrounding the hair follicles deep within the dermis. In deep (full thickness) burns, the skin is destroyed down to and including the dermis and looks white or charred, is painless and involves hair follicles, hence skin grafting is often required. Deep burns need assessment and treatment in hospital. • Surface area of the burn. This should be calculated from a surface area chart (Fig. 7.5). The palm and adducted fingers cover about 1% of the body surface. Burns covering more than 5% full thickness and 10% partial thickness need assessment by burns specialists. Involvement of more than 70% of the body surface carries a poor chance of survival. • Involvement of special sites. Burns to the face may be disfiguring, those to the mouth may compromise the airway from oedema, and those to the hand/joints may cause functional loss from scarring. Burns to the perineum and other special sites should all be referred to a burns unit. • relieving pain, assessed with a pain score; may require the use of strong analgesics such as intravenous morphine • treating shock with intravenous fluids, preferably plasma expanders, and close monitoring of haematocrit and urinary output. Children with more than 10% burns will require intravenous fluids • providing wound care. Burns should be covered with cling film (plastic wrapping), which reduces pain from contact with cold air and reduces the risk of infection. Blisters should be left alone. Irrigation with cold water should only be used briefly to superficial or partial thickness burns covering less than 10% of the body as it may rapidly cause excessive cooling. Tetanus immunisation status must be ascertained and a booster given if required. Ongoing care involves removal of dead tissue and placement of sterile dressings. Wound management is as important as antimicrobials in preventing infection: • Copious wound irrigation, toilet and debridement • Delayed wound closure, especially on limbs, due to increased incidence of infection • Prophylactic antibiotics if wounds or child is at increased infection risk, i.e. puncture wounds, bites to hands/wrists, crush wounds with devitalised tissue, bites to genitals, child has diabetes mellitus, immunosuppression and in all bites after primary closure. The antibiotic of choice is co-amoxiclav, as this also covers Pasteurella infection. • accidental – the vast majority • deliberate self-poisoning in older children • non-accidental as a form of child abuse Although many thousands of young children are rushed to doctors’ surgeries or hospital for urgent medical attention following accidental ingestion, most do not develop serious symptoms, as they ingest only a small quantity of poison or take relatively non-toxic substances (Table 7.1). However, a small percentage of children become seriously ill and a very few children die from poisoning each year. Table 7.1 Potential toxicity in accidental poisoning in infants and young children, with some examples • The introduction of child-resistant containers – in the UK they must be used for paracetamol and salicylate preparations, and certain household products, such as white spirit; an alternative container for tablets is opaque blister packs • The reduction in the number of tablets per pack • A reduction in prescriptions of potentially harmful medicines, e.g. aspirin and iron. Clinical features that may alert one to poisoning are shown in Table 7.2; however, in young children parents usually know the identity of tablets or other poisons taken (Table 7.3). Management is outlined in Figure 7.8. Table 7.2 Table 7.3
Accidents, poisoning and child protection
Accidents
Accident prevention
Head injuries
Internal injuries
Burns and scalds
Management
Treatment
Dog bites
Poisoning
Accidental poisoning
Toxicity
Medicines
Household products
Plants
Low
Oral contraceptives, most antibiotics
Chalk and crayons, washing powder
Cyclamen, sweet pea
Intermediate
Paracetamol elixir, salbutamol
Bleach, disinfectants, window cleaners
Fuchsia, holly
High
Alcoholic drinks, digoxin, iron, salicylate, tricyclic antidepressants
Acids, alkalis, petroleum distillates, organophosphorus insecticides
Deadly nightshade, laburnum, yew
Management
Tachypnoea
Aspirin, carbon monoxide
Slow respiratory rate
Opiates, alcohol
Hypertension
Amphetamines, cocaine
Hypotension
Tricyclics, opiates, β-blockers, iron (secondary to shock)
Convulsions
Tricyclics, organophosphates
Tachycardia
Cocaine, antidepressants, amphetamines
Bradycardia
β-blockers
Large pupils
Tricyclics, cocaine, cannabis, amphetamines
Small pupils
Opiates, organophosphates
Poison
Adverse effects
Management
Alcohol (accidental or experimenting by older children)
Monitor blood glucose.
Intravenous glucose if necessary.
Blood alcohol levels for severity
Acids and alkalis
Inflammation and ulceration of upper gastrointestinal tract leading to stenosis
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access