Fig. 1
The jugular vein, subclavian vein, and associated anatomic landmarks (Source: Christopher Coppola)
(c)
Subclavian: Patient is positioned supine, with Trendelenburg, and a roll between the shoulder blades. Sonography is used to identify the subclavian vein. Shoulder and neck are prepped and alcohol and sterile technique used. Vein is accessed with a needle and syringe by entering skin lateral to the site where the clavicular head of the pectoralis muscle attaches to the curve in the clavicle. Needle is kept parallel to the floor, the tip is allowed to contact the clavicle, and then is redirected between the clavicle and the first rib until the subclavian vein is entered and venous blood can be withdrawn. Aim the tip of the needle at the manubrium or larynx. Avoid directing the needle toward the floor as this will increase the chance of pneumothorax. Using Seldinger technique, the catheter is placed, ensuring that the wire is completely removed. Fluoroscopy during procedure verifies the wire is directed to the superior vena cava and not to the opposite arm or up into the neck. An 11 blade scalpel and a dilator widen the entry so the catheter can enter. Catheter is secured and dressed, then chest x-ray is performed to verify placement in the superior vena cava and ensure there is no pneumothorax.
(d)
Femoral: Patient is placed in supine position. Femoral vein is located with sonography and note is taken of the femoral artery, lateral to the vein. After sterile preparation and drape, vein is accessed with a needle and syringe, at a downward angle with needle parallel to the vein. When vein is entered, using Seldinger technique a wire is inserted into vein and is used to advance a catheter into the femoral vein. The wire is removed. It is verified that the catheter can withdraw and flush, and it is secured with a drain stitch and occlusive dressing.
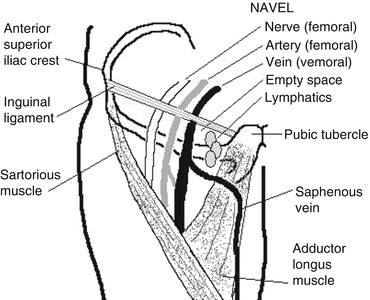
Fig. 2
Femoral artery, vein, and associated landmarks (Source: Christopher Coppola)
2.
Cut-down:
(a)
Jugular:
(i)
Technique: Patient is positioned as for percutaneous access. The space between the sternal and clavicular heads of the sternocleidomastoid muscle is palpated. A transverse incision is made a finger breadth above the clavicle. The subcutaneous tissue and platysma are separated and wound is deepened until carotid sheath is encountered. The internal jugular vein is identified. It is carefully separated from the carotid artery and the vagus nerve. Proximal and distal control of the vein is obtained by circumferential dissection and encircling vein with a 4–0 absorbable ties above and below the planned point of vein entry. The distal vein is ligated. Venotomy is created. Catheter is inserted and advanced until the tip lies within the superior vena cava. The proximal tie is tied down ensuring that it does not crush the catheter. After verifying that the catheter withdraws blood and flushes saline, the wound is closed in layers of absorbable suture. The catheter is secured to skin and covered with an occlusive dressing.
(ii)
Alternatives:
1.
The internal jugular does not necessarily need to be ligated during catheter placement. A purse string of 4-0 polypropylene suture can be used to secure the edge of the venotomy, which is then tied down around the catheter, preserving jugular flow from the head.
2.
A branch of the internal jugular, the facial vein, can be used as the entry point for the catheter, and the internal jugular will not need to be ligated.
3.
In larger children, the external jugular can be used for placement. After proximal and distal control is obtained, catheter is inserted via venotomy and must be guided into external jugular, which leads to the subclavian, and then enters the superior vena cava, via the innominate vein if on the left side.
(b)
Femoral: Cut-down is usually performed parallel and just inferior to the inguinal ligament, but a vertical incision is an alternative. From lateral to medial, the orientation of structures in the femoral triangle are Nerve, Artery, Vein, Empty space (occupied by fat), and Lymphatics (NAVEL). The femoral vein is identified, dissected out circumferentially and secured with ties proximally and distally. Catheter is inserted via venotomy. Flow in the femoral vein is preserved.
(c)
Saphenous vein runs from ankle to groin, on the medial surface of both legs. It is found easiest at the ankle, where a transverse incision is made a finger breadth superior and anterior to the medial malleolus. The vein is identified, isolated with proximal and distal control, distal vein is ligated, and catheter is inserted through venotomy, then proximal ligature is tied down to secure vein around catheter. Saphenous vein can also be found two finger breadths inferior and posterior to the femoral vein at the inguinal ligament.
3.
Peripherally inserted central catheter (PICC): A PICC line offers the advantages of a central line, since the tip lies in the superior vena cava, but with fewer mechanical and infectious complications. The best vein for PICC insertion is the basilic vein above the antecubital fossa. The vein is identified with the help of sonography. Distance from entry site to the upper chest along path of venous return is measured to estimate length of catheter that will be required. Tourniquet is applied above entry site. Vein can be accessed by percutaneous technique or cut-down. Vein is accessed by a breakaway needle that splits in half, or a short catheter, large enough to pass the PICC line, depending on which type of kit is available. PICC is inserted through this device into vein. Tourniquet is removed. PICC line is advanced until the tip reaches the superior vena cava
4.
Intraosseous (IO):
(a)
Indications and use: An intraosseous line is a useful rescue when an intravenous line cannot be obtained. In an emergency, an intraosseous line should be placed when three attempts have been made or 90 s have passed without progress. Line can be used for IV fluid, medications, transfusion, and phlebotomy. It can be started easily on children up to age 6 years old, above that age, entry into bone can be difficult without specialized devices.
(b)
Get Clinical Tree app for offline access

Devices:
(i)
Hand-driven device with detachable handle: Cook Intraosseous, threaded and smooth needles, (Cook Medical, Bloomington, IN); Jamshedi 15 g, (CareFusion, San Diego, CA)
(ii)




Battery powered drill: EZ-IO, (Vidacare, San Antonio, TX)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


