The Third Stage of Labour, from the delivery of the child until the expulsion of the placenta, remains the most unpredictable and dangerous stage of labour from the mother’s point of view.
RETAINED PLACENTA
CAUSES
1. Placenta separated but undelivered
2. lacenta partly or wholly attached

TREATMENT




PRIMARY POSTPARTUM HAEMORRHAGE
CAUSES




Abnormalities of the Third Stage of Labour and of the Placenta and Cord
The first part of this chapter describes two relatively common third stage complications, retained placenta (1–2%) and primary postpartum haemorrhage (PPH 3–4%) and the rare, but very grave, complication of inversion of the uterus. The chapter concludes with an account of some of the commoner abnormalities of the placenta and cord.
When Syntometrine has been given as described in Chapter 11, with the crowning of the head or the delivery of the anterior shoulder, separation of the placenta will usually occur within a few minutes of the delivery of the baby. Certainly, if the placenta is undelivered at 20 minutes it should be considered to be ‘retained’.
In such cases there have usually been signs of placental separation – bleeding, alteration of the shape of the uterus, lengthening of the cord. If the signs have been missed, bleeding into the uterine cavity will occur because the uterus cannot retract fully until it is empty. The fundus will therefore appear broad and boggy, thus disguising the fact that separation has occurred. Failure to recognise the signs of separation is one of the commonest forms of mismanagement of the third stage.
In this situation the fundus should be rubbed up to make it contract and the placenta removed by the Brandt–Andrews method. The cord is pulled gently, and the other hand presses the uterus upwards so as to prevent inversion. A slight seesawing motion is imparted by both hands, and provided separation has occurred the placenta should be delivered. It is likely to be accompanied by a considerable volume of accumulated blood.
Partial separation will cause bleeding but the fundus will remain broad because the placenta still occupies the upper segment. Needless handling of the uterus during the third stage is thought to encourage partial separation.
Where oxytocics have been given an hourglass constriction may develop in the lower segment and the cervix begins to close down.
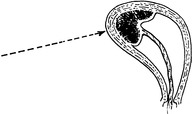
3. Placenta accreta is a rare cause of retained placenta. There is abnormal adherence of the placenta to the uterine muscle due to a defect of decidual formation. It is usually partial, and presents by partial separation accompanied by bleeding. On rare occasions it is complete, and bleeding is absent. Attempts at manual removal open the blood sinuses, causing severe bleeding, and hysterectomy may be necessary.
Placenta accreta should be suspected when the operator has difficulty in finding the plane of cleavage when attempting manual removal. The placenta may be left in utero if there is no bleeding, but infection is inevitable. Probably, in this rare condition, hysterectomy is the safest course.
This should not be delayed because of the risk of haemorrhage from partial separation. The procedure itself, however, is not without risk from infection and damage to the uterus.
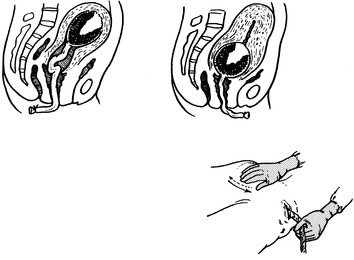
1. The hand covered with antiseptic cream is introduced into the vagina, following the cord.
2. The fingers begin to separate the placenta from the uterine wall. Never grasp the placenta until it is separated.
3. Note that the abdominal hand presses the uterus into the placenta and prevents tearing of the lower segment.
4. The placenta is inspected at once to see that it is complete and, if there is any doubt, the uterus is re-explored. Ergometrine or oxytocin is then given and the uterus rubbed up to make it contract.
1. Uterine Atony – the uterus, although empty, fails to contract and control bleeding from the placental site. This is the commonest and potentially most dangerous cause.
Predisposing Causes
(a) Excessive uterine distension (twins, polyhydramnios, large baby)
(b) Multiparity (fibrosis in uterine muscle).
(c) Prolonged labour (uterine inertia).
(d) Labour augmented with Syntocinon.
(e) General anaesthesia.
(f) Placenta praevia — lower segment does not contract well enough to stop bleeding.
(g) Placental abruption — the Couvelaire uterus may not contract. In addition a coagulation defect may develop and fibrin degradation products (FDPs) discourage uterine contraction.
2. Partial Separation of the Placenta — uterus is prevented from contracting.
3. Retention of Placental Fragments