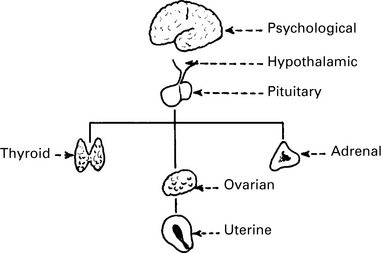
Chapter 6 Abnormalities of Menstruation
Physiological amenorrhoea
Menopause
The menopause is the cessation of menstruation (mean age 51 y) due to exhaustion of the supply of ovarian follicles. Oestrogen production therefore falls. This fall in oestrogen production is accompanied by a rise in follicle stimulating hormone (FSH) levels, which continues for a considerable time. In a proportion of women, menstruation ceases abruptly, but in many, the menstrual cycles alter. Frequently, they become shorter initially, but later they lengthen and tend to be irregular, before ceasing entirely. This phase is known as the menopause transition, and the final period is recognised only in retrospect, after 1 year of amenorrhoea. See Chapter 18.
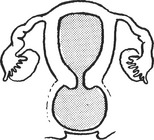
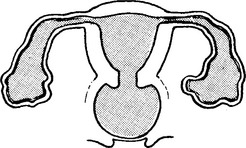
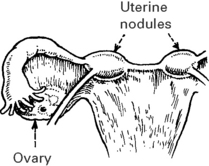
Uterine and lower genital tract disorders
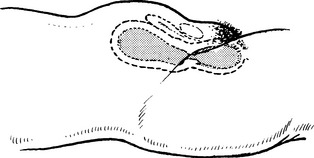
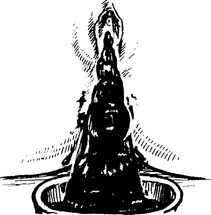
Imperforate hymen or transverse vaginal septum
Examination
A pelvic mass is palpated and may even be visible. The vaginal membrane or hymen is bulging.
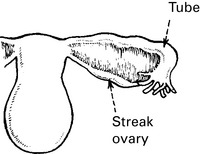
Ovarian disorders
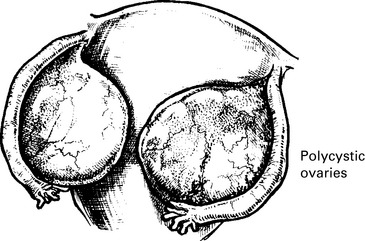
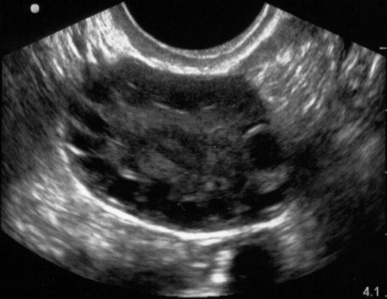
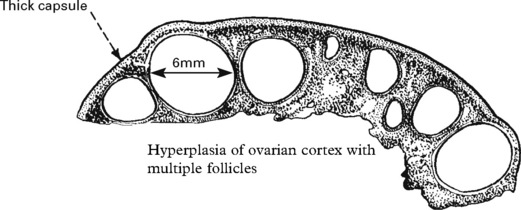
Polycystic ovarian syndrome
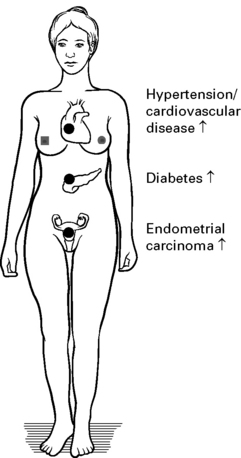
Long-term Effects of PCOS
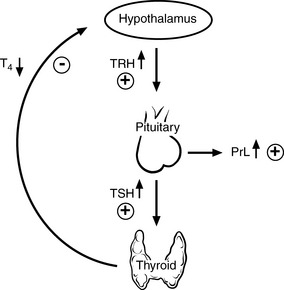
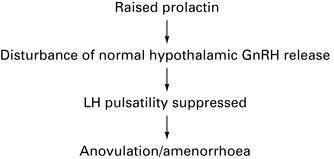
Pituitary disorders
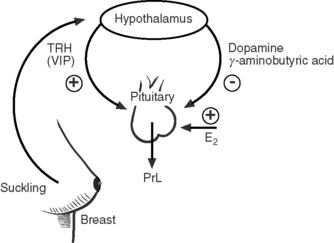
Hyperprolactinaemia
Aetiology