CHAPTER 13 dilatation of the aorta equal to or exceeding 3 cm in diameter; also known as AAA. a localized widening or dilatation of a blood vessel. an abnormal connection between an artery and vein; also known as arteriovenous shunting. small saccular aneurysms primarily affecting the cerebral arteries. a saccular dilatation of a blood vessel caused by a bacterial infection. • Arteries and arterioles carry oxygenated blood away from the heart. • Veins and venules carry blood toward the heart. • Capillaries connect the arterial and venous systems. • Extremity veins contain valves. • Valves extend inward toward the intima. • Originates at the diaphragm and courses inferiorly until it bifurcates into the right and left common iliac arteries. • Tapers in size as it courses anterior and inferior in the abdomen. • Common iliac arteries are the terminal branches of the abdominal aorta. • Common iliac artery bifurcates into the external and internal (hypogastric) iliac arteries. • External iliac artery becomes the common femoral artery after passing beneath the inguinal ligament. • Internal iliac artery bifurcates into anterior and posterior divisions. • First major branch of the abdominal aorta. • Arises from the anterior aspect of the aorta. • Branches into the splenic, left gastric, and common hepatic arteries. • Low-resistance blood flow, with continuous forward flow in diastole. • Second major branch of the abdominal aorta. • Arises from the anterior surface of the aorta, inferior to the celiac axis. • Courses inferiorly and parallel to the aorta. • Branches supply the jejunum, ileum, cecum, ascending colon, portions of the transverse colon, and the head of the pancreas. • High-resistance multiphasic blood flow when fasting. • Low-resistance elevated systolic and diastolic velocities, with continuous forward flow in diastole following a meal. • Distance from the anterior wall of the aorta to the posterior wall of the SMA should not exceed 11 mm. • Right renal artery arises from the anterior lateral aspect of the abdominal aorta. • Left renal artery arises from the posterior lateral aspect of the abdominal aorta. • Located 1.0 to 1.5 cm inferior to the superior mesenteric artery. • Course posterior to the renal veins. • Right side arises superior to the left and courses posterior to the inferior vena cava. • Renal artery bifurcates into segmental arteries at the renal hilum. • Renal artery gives rise to the inferior suprarenal artery. • Low-resistance blood flow, with continuous forward flow in diastole. • Last major branch of the abdominal aorta superior to the aortic bifurcation. • Arises from the anterior aorta. • Courses inferior and to the left of midline. • Supplies the left transverse colon, descending colon, upper rectum, and sigmoid. • Source of collateral flow to the lower extremities. • Visualized on ultrasound in an oblique plane, slightly to the left of midline and approximately 1 cm superior to the aortic bifurcation. • Low-resistance blood flow, with continuous flow through diastole. • Arises from the anterior aspect of the abdominal aorta branching into the right and left inferior phrenic arteries just below the diaphragm near the level of the 12th thoracic vertebrae. • Supplies the inferior portion of the diaphragm. • Branch of the common hepatic artery. • Lies between the superior portion of the duodenum and the anterior surface of the pancreatic head. • Common hepatic artery is a branch of the celiac axis. • Gives rise to the gastroduodenal artery and is now termed the proper hepatic artery. • Proper hepatic artery gives rise to the right gastric artery. • Courses adjacent to the portal vein. • The proper hepatic artery bifurcates into the right and left hepatic arteries at the hepatic hilum. • The right hepatic artery gives rise to the cystic artery to supply the gallbladder. • Low-resistance blood flow, with continuous flow through diastole. • Increased flow velocity is associated with jaundice, cirrhosis, lymphoma, and metastases. • Formed at the junction of the right and left common iliac veins. • Carries oxygen-depleted blood from the body superiorly to the right atrium of the heart. • Major abdominal branches include lumbar veins, right gonadal vein, renal veins, right suprarenal vein, inferior phrenic vein, and hepatic veins. • Drain blood from the lower extremities and pelvis. • Formed by the junction of the external and internal iliac veins. • Course anterior to the renal arteries. • Left renal vein courses posterior to the superior mesenteric artery and anterior to the abdominal aorta. • Left renal vein receives the left suprarenal and gonadal veins. • Left renal vein may appear dilated because of compression from the mesentery. • Right renal vein has a short course to drain into the lateral aspect of the IVC. • Lie at the boundaries of the hepatic segments (intersegmental) and course toward the IVC. • Three major branches: left, middle, and right hepatic veins. • Right hepatic vein courses coronally between the anterior and posterior segments of the right hepatic lobe. • Middle hepatic vein follows an oblique course between the left and right hepatic lobes. • Left hepatic vein courses posterior between the medial and lateral segments of the left hepatic lobe. • Doppler demonstrates spontaneous, multiphasic, and pulsatile blood flow toward the IVC (hepatofugal). • Increase in blood flow with inspiration and diminished flow with Valsalva maneuver. • Drains the gastrointestinal tract, pancreas, spleen, and gallbladder. • Provides approximately 70% of the liver’s blood supply. • Formed by the junction of the splenic and superior mesenteric veins. • Bifurcates into the right and left portal veins just beyond the porta hepatis. • 1.3 cm in diameter in adults greater than 20 years of age. • 1.0 cm in diameter between 10 and 20 years of age. • Demonstrates phasic low-flow velocities toward the liver (hepatopetal). • Blood flow will decrease with inspiration and increase with expiration. • Diameter will increase after a meal. • Additional tributaries include: • Joins the superior mesenteric vein to form the main portal vein. • Courses posterior to the pancreas and crosses anterior to the superior mesenteric artery. • Demonstrates spontaneous phasic flow away from the spleen and toward the liver. • Normal adult diameter is 10 mm or less. • Increase in caliber with inspiration. • Drains the spleen, pancreas, and a portion of the stomach.
Abdominal vasculature
Physiology and anatomy
Functions of the vascular system
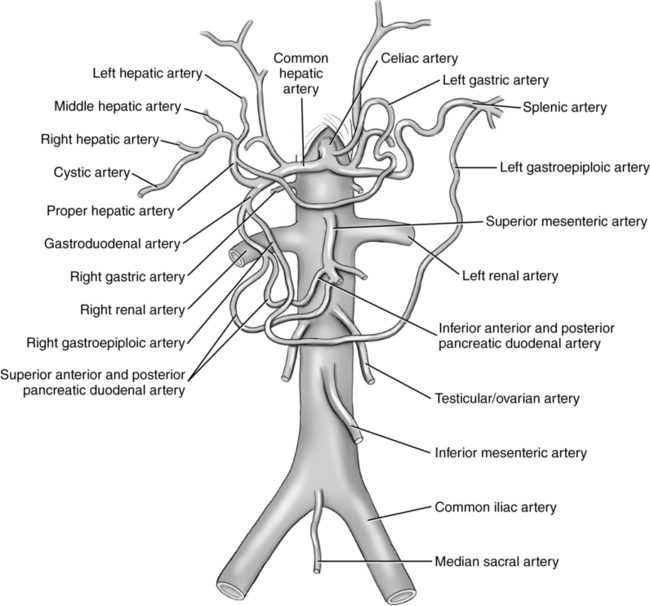
Arterial anatomy (fig. 13-1)
Abdominal aorta
Main visceral branches of the abdominal aorta
Celiac axis (CA)
Superior mesenteric artery (SMA)
Main renal arteries
Inferior mesenteric artery
Main parietal branches of the abdominal aorta
Inferior phrenic artery
Additional abdominal arteries
Gastroduodenal artery (GDA)
Hepatic artery
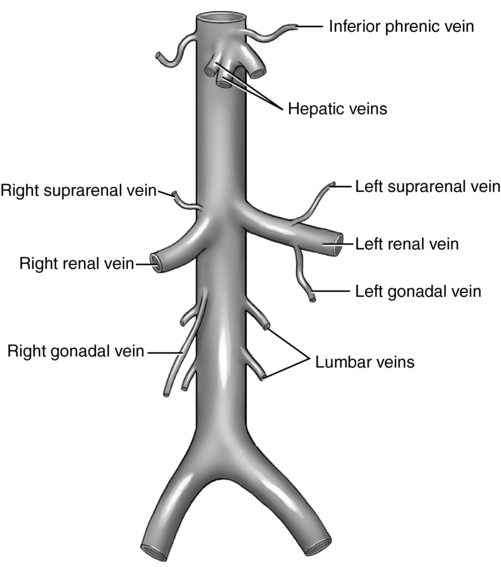
Venous anatomy (fig. 13-2)
Inferior vena cava (IVC)
Main venous tributaries
Common iliac veins
Renal veins
Hepatic veins
Additional abdominal veins
Main portal vein
Splenic vein
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Abdominal vasculature