Vaccination technique
- It is important to minimise anxiety, distress and pain associated with injected immunisations.
- Use age-appropriate pain-reduction techniques; refer to chapter 4, Pain, p. 61. These might include:
– Distraction techniques: passive (watching a toy) or active (blowing bubbles).
– Rewards (stickers or new book).
– A variety of pharmacological agents have been shown to attenuate immunisation pain (oral sucrose in infants, topical anaesthetic agents, etc.).
- Use a new syringe and needle for each injection.
- Use a 23-gauge needle, 25 mm in length. Smaller gauge needles (25-gauge) may be used for the 2 month injections for premature babies; for subcutaneous injections into the upper arm; or for intradermal (e.g. BCG) vaccinations.
- All intramuscular vaccines should be injected deep into a muscle. Insert needle at an angle of 70–90° into the anterolateral thigh and pointing towards the knee (<12 months of age) or into the deltoid pointing towards the shoulder (≥12 months of age).
- Multiple vaccines: two injectable vaccines can be given into the same limb, separated by >25 mm.
- Ensure safe and effi cient vaccination:
– Cold chain: Never use a vaccine if there is any doubt about its safe cold chain storage. Vaccines should be kept in a refrigerator reserved for vaccine/medicine storage at 2–8°C and never frozen.
– Prevent immunisation errors: Always maintain a high standard of systematic checking to reduce the chance of errors.
– Post-vaccine observation: Recipients of any vaccine should remain in the vicinity of medical care for approximately 15 min. Although anaphylaxis is very rare, it can occur with any vaccine. I.m. adrenaline must be available and given urgently in this situation; refer to chapter 1, Medical emergencies, p. 6.
Common misconceptions for missing vaccinations
Children may be under-immunised for their age when health professionals miss opportunities to vaccinate, when parents forget/miss appointments or when parents actively oppose vaccination. Only 1–2% of parents refuse vaccination for their children because they oppose vaccination. Some common misconceptions about vaccination include:
- Natural infection is the best way to achieve immunity.
- Vaccination weakens the immune system.
- ’Homeopathic immunisation’ is safer and more effective.
It is essential to address parents’ concerns, to emphasise the well-established risks associated with not vaccinating their child and to provide reassurance about vaccine safety. The back cover of The Australian Immunisation Handbook has an invaluable table for immunisation providers and parents comparing the effects of vaccines and diseases. This table compares the range and rate of disease effects, and the range and rate of vaccine side effects. This table also appears on the back of the parent-checklist sheet that is given to each family when their child is having a vaccine.
Contraindications to vaccination: true and false
Table 9.1 False contraindications to vaccination
| Usually, children should still be vaccinated, even if they: |
| • Have a cold, or low-grade fever (<38.5°C). |
| • Have a family history of any reactions following vaccination. |
| • Have a family history of convulsions. |
| • Have a history of pertussis-like illness, measles, rubella or mumps infection. |
| • Are premature (vaccination should not be postponed). |
| • Have a stable neurological condition such as cerebral palsy or Down syndrome. |
| • Have been in contact with an infectious disease. |
| • Have asthma, eczema, or hay fever. |
| • Are on antibiotics. |
| • Are on locally acting (inhaled or low-dose topical) steroids. |
| • Have a pregnant mother. |
| • Are being breast-fed. |
| • Have had recent or imminent surgery. |
| • Are of low weight but otherwise healthy. |
(Adapted from The Australian Immunisation Handbook, 9th edition).
Table 9.2 Contraindications to vaccination
| All vaccines | Acute febrile illness (if fever >38.5°C, postpone vaccination) Previous anaphylaxis contraindicates further dosage of the same vaccine |
| DTPa | Encephalopathy within 7 days of previous DTP vaccination* |
| Live vaccines (e.g. MMR, varicella) | Usually contraindicated in immunosuppressed children, e.g. chemotherapy or high-dose corticosteroids (2 mg/kg per day for >1 week). |
| MMR and varicella vaccines should be deferred if <3 months after injection of a blood product (immunogenic response may be diminished) | |
| MMR and varicella should be given on the same day or separated by 1 month (this does not apply to any killed vaccines) | |
| Other vaccines | Severe adverse reactions (extremely rare) |
* defined as severe acute neurological illness with prolonged seizures and/or unconsciousness and/or focal signs not due to another identifi ed cause.
Table 9.3 Current vaccines, their abbreviations and available forms with trade names
| Disease | Vaccine | Available products |
| Hepatitis B | hepB | Engerix-B, H-B VaxII |
| Diphtheria, tetanus, pertussis, hepatitis B, Haemophilus influenzae type B, polio | DTPa-hepB-Hib-IPV | Infanrix-hexa |
| Diphtheria, tetanus, pertussis, polio | DTPa-IPV | Infanrix-IPV |
| dTpa-IPV | Boostrix-IPV | |
| Diphtheria, tetanus, pertussis | dTpa | Boostrix, Adacel |
| Diphtheria, tetanus | dT | ADT Vaccine |
| Haemophilus influenzae type B | Hib (PRP-OMP) | Pedvax HIB |
| Hib (PRP-T) | Hiberix | |
| Haemophilus influenzae type B, hepatitis B | Hib (PRP-OMP)-hepB | Comvax |
| Poliomyelitis | IPV | IPOL |
| Measles, mumps, rubella | MMR | MMR II, Priorix |
| Measles, mumps, rubella, varicella | MMR, VZV | ProQuad, Priorix-Tetra |
| Varicella | VZV | Varilrix, Varivax |
| Influenza | Infl uenza vaccine | Vaxigrip, Fluvax, |
| Fluad, Fluarix, | ||
| Fluvirin, Influvac | ||
| Pneumococcal disease | 23-valent pneumococcal polysaccharide vaccine (23vPPV) | Pneumovax 23 |
| 7-valent pneumococcal conjugate vaccine (7vPCV) | Prevenar | |
| Meningococcal C disease | Meningococcal C conjugate vaccine (MCCV) | Meningitec, Neis-Vac, Menjugate |
| Meningococcal disease A, C, W, Y | Meningococcal vaccine polysaccharide | Mencevax, Menomune |
| Human papillomavirus | HPV 4-valent vaccine | Gardasil |
| HPV bivalent vaccine | Cervarix | |
| Rotavirus | Rotavirus vaccine | Rotarix, RotaTeq |
The Australian standard vaccination schedule 2008
Table 9.3 indicates current vaccines, their abbreviations and available forms with trade names. The NHMRC recommends an antigen-based vaccination schedule. Although vaccine antigens to be given are the same throughout Australia, the schedule differs slightly in different states of Australia as states purchase different combination vaccines. The Australian schedule, at March 2008, is shown in Table 9.4. Schedules applicable to other states are available in The Australian Immunisation Handbook, 9th edition.
- Premature infants born <32 weeks and infants born <2000 g require an additional HepB vaccine at 12 months.
- Premature infants born <28 weeks, infants born >28 weeks with chronic long disease and children with specific underlying medical conditions (see Pneumococcal vaccines, p. 116) require a fourth conjugate pneumococcal vaccine at 12 months and 23-valent polysaccharide pneumococcal vaccine at 4 years.
- Varicella vaccine is funded for infants aged 18 months. It can be given at 12 months of age on the same day as MMR vaccine or 4 weeks later.
- Catch-up varicella vaccine is given to students in Year 7 who have not had chickenpox or varicella vaccine.
- Adolescents aged 11–15 years who have not previously had hepatitis B vaccine are given 2 doses 4–6 months apart (using adult formulation).
- Infl uenza vaccine can be given to any infant ≥6 months. Children in certain risk groups are highly recommended annual influenza vaccine. Children <9 years require two doses in the fi rst year they receive the vaccine. Doses vary according to age: 6 months–3 years = 0.25 mL, ≥3 years = 0.5 mL.
- One brand of oral rotavirus vaccine (RotaTeq) has a third dose given at 6 months.
Catch-up doses
When infants and children have missed scheduled vaccine doses, a ‘catch-up’ schedule should be recommended. Never miss an opportunity to provide overdue immunisations or at least institute a written catch-up plan. Sometimes the catch-up schedule is relatively simple to devise, e.g. the 2, 4 and 6 month vaccines can be given 1 month apart, hence a late 2 month vaccine given at 3 months can be followed by the routine 4 month vaccines just 1 month later at 4 months. Catch-up schedules for newly arrived immigrants can be complex; see chapter 10, p. 127 and the RCH website. Comprehensive catch-up doses according to the overdue vaccine are clearly covered in The Australian Immunisation Handbook, 9th edition.
Table 9.4 Australian Immunisation Schedule (from 1 March 2008)
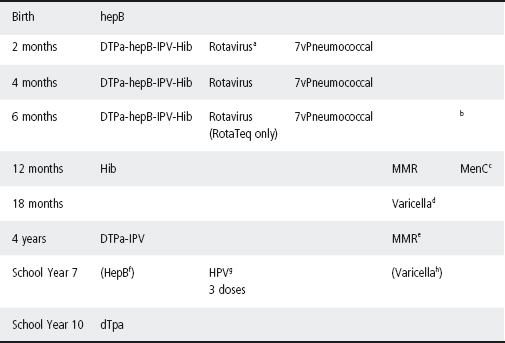
a RotaTeq, 2 mL at 2, 4 and 6 months of age. Rotarix, 1 mL at 2 and 4 months only. Minimum interval between doses is 4 weeks. Oral rotavirus vaccine is not recommended beyond the following age limits owing to limited safety data at older ages: RotaTeq 1st dose by 12 weeks of age and 3rd dose by 32 weeks of age, Rotarix 1st dose by 14 weeks of age and 2nd dose by 32 weeks of age.
b Influenza vaccine can be given to infants ≥6 months. Children in certain risk groups are highly recommended annual influenza vaccine. Children <9 years require two doses in the first year they receive the vaccine spaced ≥4 weeks apart. Doses vary according to age: 6 months–3 years 0.25 mL, >3 years 0.5 mL.
c Meningococcal C conjugate vaccine can be given <1 year but is not funded (2–6 months 3 doses; 6–12 months 2 doses).
d Varicella vaccine is funded for infants aged 18 months. It can be given at 12 months of age on the same day as MMR vaccine or 4 weeks later.
e MMR vaccine second dose can be given at 18 months.
f Catch-up hepatitis B vaccine is given to adolescents aged 11–15 years who have not had hepatitis B vaccine. Two doses 4–6 months apart (using adult formulation).
g Catch-up HPV vaccine is funded for girls aged 12–26 years until mid-2009. The funding will then be ongoing for girls in Year 7. Three doses spaced 0, 2 and 6 months.
h Catch-up varicella vaccine is given to students in Year 7 who have not had chickenpox or varicella vaccine.
The RCH immunisation service
Healthcare providers often encounter problems as the immunisation schedule changes regularly, catch-up doses can be diffi cult to work out and families sometimes have complex questions. The RCH Immunisation Service assists doctors, immunisation providers and parents through its telephone service (03 9345 6599) and weekly outpatient clinics for discussion of individual cases. There is a drop-in centre at the hospital to assist in provision of opportunistic immunisations for inpatients and outpatients.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


