Definition of developmental biomechanics 48
Introduction 48
Summary 81
Definition of developmental biomechanics
The study of the effects of externally applied forces on the musculoskeletal system during early life.
Introduction
This chapter does not provide the reader with an exhaustive account but rather attempts to provide an overview of the gross morphological development of the lower limb and foot from birth to maturity, so that these notable aspects of development of the lower limb and foot can be appreciated in such a way that useful clinical benchmarks ensue.
Clearly, it is only by understanding the normal development of the lower limb that clinical abnormalities can be distinguished from developmentally expected parameters. A classic example of the importance of this distinction occurs at the knee, where genu varum is clinically normal in an infant aged 6 months, yet clinically abnormal in a child aged 4 years. Knowledge of developmental traits and variants are essential for the clinician in both the detection of problems and an appreciation of normal physiologic growth. Tempering the need for clinical benchmarks is the appreciation that a wide spectrum of ‘normal’ is encountered.
Spine
The newborn spine is kyphotic, with the vertebral column from cervical to sacral level being a continuous flexion curve (as viewed laterally). The proportions of the segments of the spine are vastly different to those of the adult, with the cervical and lumbar lengths approximating some 25% each of the total length.
Imaging the young spine
Spinal sonography can be performed in newborns and young infants as long as the vertebral arches are not completely ossified. Indications for spinal sonography are midline cutaneous markers in the lumbosacral region, subcutaneous masses, foot abnormalities, anorectal and genitourinary malformations and neurological abnormalities of the lower extremities. All these clinical symptoms are suspicious of spina bifida occulta and tethered cord which should be ruled out by spinal sonography (Deeg et al 2007).
Sonography of the neonatal spine is now accepted as a highly sensitive, readily available screening study that can be used to evaluate various anomalies of the lumbar spine in most infants younger than 4 months (Lowe et al 2007). Fetal magnetic resonance imaging (MRI) is an increasingly available technique used to evaluate the fetal brain and spine. This is made possible by recent advances in technology and it affords a unique opportunity for studying in vivo brain development and early diagnosis of congenital abnormalities inadequately visualized or undetectable by prenatal sonography (Glenn & Barkovich 2006).
Working against gravity
Development of the neuromuscular system results in many antigravity motions of the infant which has the net effect of mobilizing the spine from flexion to extension. These movements should be occurring and actively observable by 6 months of age (Fig. 4.1).
Key Concepts
Key Concepts
It is important to appreciate the concept that modelling of bony structures is a dynamic process. Fed by the maturation of the neurological system, muscle activity and resulting movements direct forces across young bones and joints to direct eventual morphological form (Guidera et al 1994).
Students might like to remember the following motto:
‘It’s the nerves, which drive the muscles, to shape the bones.’
Typical movements and ages at which these emerge are:
| •Head lift: | 2 months (asymmetrical). |
| •‘Frog leg’ and kick: | 3 months. |
| •‘Swimming’: | 4–5 months. |
| •Tummy crawl: | 6 months. |
| •Quadruped rock: | 7 months. |
It is important for the prone and supine skills to be balanced, which has important implications for positioning the infant.
Sudden infant death syndrome (SIDS)
Parents in the 1950s were very influenced by the manual for babies and infants written by Dr Benjamin Spock. Parents were advised to lie babies prone for sleeping, a practice which was later identified as being associated with SIDS and is now warned against. The practice of lying babies supine has altered motor development by delaying the attainment of skills gained from prone positioning. Plagiocephaly is also more common and children’s health clinics now advocate regular ‘tummy time’ when babies are awake to build strength from prone posture. The risk for sudden infant death syndrome in black infants is twice that of white infants, and their parents are twice as likely to place them in the prone position for sleep (Colson et al 2006, Moon et al 2004).
On their feet
The newly standing and, in many cases, walking 1-year-old child displays an anterior pelvic tilt. Adjustment of the pelvic tilt allows for centre of gravity adaptation with growth, ranging from 18 to 40° (iliac crest angulation to transverse plane).
The typical ‘pot belly’ appearance of the 2-year-old child occurs due to lumbar hyperextension in combination with anterior pelvic tilt. This continues to form a structural lumbar lordosis which counterbalances with developmental genu recurvatum in the 2–3-year-old child.
Lordotic curvature in the lumbar region increases during ages 4–7 years, reaching the maximal value of approximately 30–40° anterior pelvic tilt by 7 years. Tightness of structures such as the hamstrings may result in a greater than usual anterior pelvic tilt or may see the degree of pelvic tilt reached at an earlier age. This is more marked in children with muscular hypertonicity (Fig. 4.2). Referral to either a physiotherapist or an orthopaedist for more comprehensive assessment may be indicated, and is also indicated with observation of other asymmetry, such as one very pronated foot versus a normal foot (functional limb length discrepancy). Subtle asymmetry does not necessarily require intervention.
 |
| Figure 4.2 |
Pelvic tilt and lumbar lordosis, two position-dependent factors, increase with age, to avoid inadequate anterior displacement of the body centre of gravity (Mac-Thiong et al 2004).
Pelvis
The newborn pelvis is small and tilted posteriorly in the sagittal plane, even more so when the infant is positioned prone.
The acetabular cup is shallow and faces inferiorly in the sagittal plane. By 3 years of age the acetabular cup angles further inferiorly.
The hip joint is in a position of flexion and lateral rotation due to the combined forces of surrounding ligaments and muscles. Both capsular ligament contracture and also contracture of hip flexors and lateral rotator muscles are involved in this posture. There are twice as many lateral rotators as medial rotators at the hip joint.
The posture of the newborn baby reflects the ‘close packed’ position in utero in the last trimester of pregnancy (Fig. 4.3). Note the flexion/abduction of hips, knee flexion, medial tibial position, ankle dorsiflexion, relative adduction of the feet. The stress of this close packed positioning stabilizes joint complexes. The rapidly increasing size of the fetus from 22 to 24 weeks’ gestation means that the available space for the developing body becomes diminished, necessitating the closely wrapped position of flexion of most joints. Thus, post-birth, the direction of musculoskeletal development is one which reduces this flexed and tightly packed posture to one which in approximately 10–16 months sees the child extended and bipedal.
Around the hip joints we see the necessary reduction of flexion and lateral rotation (the infant is no longer physically confined) due to the activation of muscle groups and the simultaneous stretching of ligaments. Together these forces shape the osseous structures. The following brief and very simplified description in relation to the hip may assist in understanding the basic concepts of this bony modelling process:
• the acetabular cup deepens and angles more inferiorly
• due to the force of placement of the head of femur
• which is moved ‘into’ the acetabulum
• following the end of intrauterine confinement, activation of hip extensors, elongation of anterior pelvic capsular ligaments.
The aim of this process is to produce a stable hip joint for eventual bipedal weight-bearing. It is important to remember that the maturation of the nervous system sees activity occurring in the muscles, which through their agonist–antagonist pairing, place modelling forces through young plastic bones and ligaments, resulting in the eventual skeletal form. Postures in the infant may also be influential to a lesser degree on eventual skeletal form and often have cultural association (e.g. swaddling with legs extended versus carrying on backs with abducted, flexed hips).
Developmental dysplasia of the hip (DDH)
Early detection, diagnosis and treatment of developmental dysplasia of the hip (DDH; previously known as congenital hip dislocation) are essential in preventing further disability and reduced quality of life for affected children. In a study of 8145 infants, the rate of suspected DDH was 0.95% and that of diagnosed DDH was 0.63% (Stein-Zamir et al 2008). Children with DDH have the following demographic and perinatal risk markers:
Key Concepts
• female
• first born
• breech presentation
• oligohydramnios.
Key Concepts
The highest positive predictive value (95.5%) in physical evaluation was any sign of a dislocatable hip, as assessed using Ortolani’s or Barlow’s tests (Shepherd 1995). DDH diagnosis after 6 weeks of age was associated with a higher likelihood of surgery and motor disability.
Clinical screening to enable early diagnosis of DDH is essential to avoid later problems (Fig. 4.4).
Hip joint range of motion
Hip joint range of motion is in three cardinal body planes:
1. Sagittal
At birth the hip is flexed some 30°. The iliofemoral and ischiofemoral ligaments together with the iliopsoas muscle are short and inactive and aid in this position of flexion. Gluteus maximus and the proximal portion of adductor magnus become active and antagonize these structures with their function as hip extensors.
The clinical test for hip extension range is Staheli’s prone hip extension test. From 3 years the normal hip extension is 0°, which in part accounts for the short stride length in children under 3 years (adults usually have 55° of hip extension/flexion).
Hip flexion contracture of 15–20° is an indication for surgical lengthening as approximately 15° of hip extension is required for the child to walk normally. Hip extension is an abnormal finding in gestation.
2. Transverse
Until age 2 years, the range of lateral rotation in the transverse plane at the hip joint exceeds that of medial rotation. Coupled with this change in proportion of motion is reduction in the quantity of motion, from 120–150° in the newborn to approximately 100° by age 2 years. Anteversion reduces simultaneously with antetorsion (defined below, under Femur), but involves different structures.
3. Frontal/coronal
The hip joint is abducted 75° in the neonate (while flexed) and this is reduced to 60° by approximately 9 months of age. In the 2-year-old child the normal amount of hip abduction is 45°, which remains fairly static into adulthood.
Coxa valga (angle between the head/neck axis and the femoral shaft axis in the frontal plane) measures up to 150° in the neonate, reducing to its mature value of 125–135° by 6 years.
Femur
The femur is the largest bone in the body and its development is almost as contentious and confusing in terms of nomenclature.
The terms anteversion and antetorsion (and counterparts, retroversion and retrotorsion) are used with variation by many authors due to divergence of definition (Fabry et al 1994, Valmassy 1996). For the purpose of clarity we adopt the definitions of Cusick (Cusick 1990, Cusick & Stuberg 1992):
Torsion (femoral):
‘A medial twist in the shaft of the bone, distal on proximal.’
Version (femoral):
‘A positional change in which either the acetabulum or the head and neck of the femur are directed anteriorly, relative to the frontal plane. The head and neck of the femur are maintained in this alignment by soft tissue, including ligament, muscle, and joint capsule.’
There are three distinct growth plates in the proximal femur which contribute to growth:
• Longitudinal growth plate: contributes 30% to femur length.
• Trochanteric growth plate: contributes to modelling of femoral head and neck.
• Femoral neck isthmus.
The proximal femur is composed entirely of hyaline cartilage in the neonate and is thus very pliable in infancy and early childhood.
The newborn femur shows:
• coxa valga
• femoral torsion (medial)
• mild varus bowing
• some anterior bowing.
Each of these femoral attributes indicates skeletal immaturity due to intrauterine position and fetal skeletal design.
Coxa valga
Describes the angle formed between the femoral neck and shaft.
Approximates 150° in the neonate and reduces with age to 125–135° at 6 years, 125° in the adult.
Table 4.1 provides a summary of the most commonly assessed aspects of the lower limb (excluding the foot) and normative values across main research studies (Beeson 1999, Cheng et al 1991, Cusick & Stuberg 1992, Eckhoff & Johnson 1994, Fabry et al 1994, Guidera et al 1994, Heath & Staheli 1993, Jacquemier et al 2008, Kumar & MacEwen 1982, Pasciak et al 1996, Schneider et al 1997, Staheli 1989).
| *Method of assessment: CT values (torsion) approx. 10° less than TMA method. | |||||
| Hip | Femur | Knee | Tibia | Thigh–foot | |
|---|---|---|---|---|---|
| Age (years) | Position | Torsion | Position | Torsion | Angle |
| 0–2 | Medial hip range: 43° age 2 years Lateral hip range: 40° at 2 years | Average: Females: >40° medial at birth Males: 30° | Genu varum at birth averages 10°, abnormal after 2 years | Minimal at birth | Average: −10° to 0° (range −25° to 20°) |
| 3–4 | Average Females: 40° medial (SD 20°) Males: 28° (18°) | Genu valgum: maximizes with 8–12° valgus at 3–4 years | TMA averages 34° lateral (SD 6°) | 15° abducted after age 2–3 years | |
| 7–8 | Average Females: 28° medial (SD 20°) Males: 14° (14°) | Genu valgum: reduces to <5° | * Torsion averages 20° lateral (range 0–45°) by ages 7–8 years | ||
| 9–12 | Medial hip range: 56° by 9 years Lateral hip range: 30° at 9 years | Average Females: 10–15° medial by age 10 years (SD 15°) Males: 10° (14°) | Genu valgum > 10° is abnormal | * TMA averages 35° lateral (SD 4°) | Averages 10° abducted (range −5° to 35°) at age 12 years |
| Adult | 45° medial 45° lateral | 15° medial (females) 5° medial (males) | Torsion 20° TMA 35° | 10° abducted | |
Femoral torsion
Describes the medial twist in the shaft of the bone, distal on proximal end.
At birth there is approximately 40° of medial femoral torsion.
By 2 years 30° of femoral torsion remains, having reduced due to:
Key Concepts
• Reduced hip flexion contracture.
• Activation of hip extensors and lateral rotators (which put a torsional modelling force through the proximal third of the cartilaginous femur).
Key Concepts
Reduction of femoral torsion is greatest in the first 2 years (from approximately 40° to 30°) and again at puberty (from approximately 25° to 15°).
The adult femoral torsion range varies according to different studies (and individuals): 5–15° (Cusick 1990).
The mean value of femoral torsion measured using ultrasound in 97 children aged 6 and 15 years was 37° in the 6-year-old group and 24° in the 15-year-old group. The mean value of tibial torsion was 18° in both age groups. Neither side- nor sex-dependent differences in both age groups were found (Pasciak et al 1996).
Average femoral torsion measured using magnetic resonance imaging (MRI) was 10.4°. MRI provides an alternative to computed tomography (CT) in the measurement of femoral and tibial torsion (Schneider et al 1997).
Key Concepts
Key Concepts
Clinical assessment of torsion of the femur is estimated using Ryder’s test. This clinical test indirectly assesses the torsional status of the femur and has been found to demonstrate good reliability and validity in the hands of experienced examiners. It may, however, underestimate femoral torsion in some children with cerebral palsy due to altered trochanteric sites (Cusick 1990, Cusick & Stuberg 1992, Davids et al 2002; Figs 4.5, 4.6).
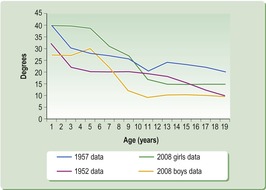 |
| Figure 4.6 This summary of two studies from the 1950s (both had over 200 subjects) identified the same trend in reducing femoral torsion with increasing age, but values varied due to hip positioning and examiner technique (Cusick 1990). The 2008 data (over 1300 children) separate girls and boys and show appreciable gender difference with greater femoral torsion as a part of the female profile (Jacquemier et al 2008). |
Knee
Similarly to the hip joint, the newborn’s knee exhibits flexion contracture as a normal finding. Accompanying this position are the attitudes of genu varum and medial genicular position.
Knee joint in three cardinal body planes
1. Sagittal plane
The knee of the neonate is flexed approximately 30° due to:
a. intrauterine positioning → adaptive shortening of soft tissues
b. maturation of the nervous system → flexor muscle activity.
These two factors combine to result in ‘physiologic flexion’ in newborns as observed in elbows, hips, ankles and knees.
Normal development sees reduction of this flexion by 6 months of age, assisted by the infant’s ‘mouthing’ of their feet, an activity which actively assists in elongating hamstrings both actively and passively. Infants continue to elongate their hamstrings and hence reduce knee flexion, by standing and later moving to begin the bear stand/walk posture.
2. Transverse plane
Flexion of the knee allows medial rotation of the tibia on the distal femur. Intrauterine confinement flexes the knee, rotating the tibiofibular unit medial to result in the medial genicular position on the newborn lower legs. There are more muscles crossing the knee medially than laterally such that flexion denotes medial rotation. There is also adaptive tightness of ligaments and joint capsule from intrauterine positioning.
The ligaments and joint capsule must stretch to allow lateral rotation of the tibiofibular unit on the distal femur as occurs with knee extension. This lateral rotation is essential for knee stability and efficient ‘locking’ and ‘unlocking’ functioning in later gait. The initial medial genicular position needs to reduce to allow for adequate lateral rotation with knee extension.
Approximately 5° of lateral rotation of the tibiofibular unit occurs in the last 10° of knee extension to make the knee congruent. Increased transverse plane range of motion in children under 3 years reflects the connective tissue and muscular mobility of this osseous unstable joint.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






