Case 23 A boy with nonspecific symptoms
Asil, a 7-year-old Turkish boy, has a fever and a runny nose. He becomes ‘lifeless and lethargic’ and is taken to the GP. His parents speak limited English so it is difficult to get a clear history. Blood tests are requested and show a normal Hb, WCC and platelet count. The CRP is 20 (normal <6 mg/L), there are atypical mononuclear cells on the blood film and the monospot is positive.
What is the likely diagnosis?
The GP makes a diagnosis of glandular fever.
A week later Asil is brought back to the GP. He has developed bad headaches which keep him awake at night despite paracetamol and ibuprofen. He is vomiting and this is getting worse. He does not have diarrhoea. The GP feels that the symptoms are compatible with glandular fever, prescribes dioralyte and reassures the family.
What should be done now?
About 3 weeks later Asil’s parents bring him to the ED one evening. Again there is a language barrier which makes obtaining the history difficult. Asil’s headaches are worse and he is still vomiting frequently. Examination by a FY2 ED doctor does not reveal any abnormalities but it is noted that Asil has lost weight, 2 kg in approximately 3 weeks. His symptoms are again thought to be due to glandular fever and he is sent home and the family are advised to continue with the analgesia and to keep Asil well hydrated.
What are your concerns at this point?
Two weeks later the GP refers Asil to the paediatric rapid referral clinic where he is seen by the consultant paediatrician. He still has headaches and vomiting. On examination Asil is miserable and thin. He is thought to be slightly dehydrated and has a central capillary refill time of 3–4 seconds. There is no fever, no lymphadenopathy and no rash. No abnormalities are detected in the respiratory or cardiovascular systems. His abdomen is scaphoid, soft and nontender. There is no organomegaly. He has no neck stiffness.
What is the differential diagnosis now?
Asil is admitted to the day unit for a fluid challenge. The plan is that if the fluid challenge fails he will require iv fluids and that blood tests will be done when the cannula is inserted. Asil has a urine dipstick which is normal and 2 hourly observations. Whilst on the day unit he vomits several times and complains of a severe headache. There is a family history of migraine.
He is examined by the paediatric ST1 who cannot see the fundi, documents that the cranial nerves are normal, finds power, tone, and coordination to be normal but thinks that the knee and ankle jerks are too brisk and that there is bilateral ankle clonus.
Asil is then examined by a registrar who confirms the pathologically brisk reflexes and the clonus in the ankles.
What should happen next?
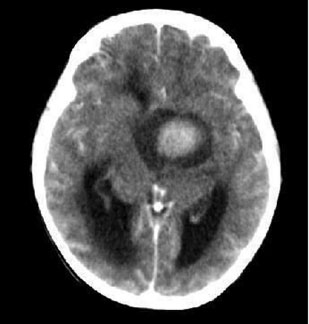
Asil has an urgent CT brain scan (Case Figure 23.1)
< div class='tao-gold-member'>