Treatment aims
- Prevent and treat burn shock.
- Provide adequate analgesia.
- Prevent infection.
- Obtain early skin cover.
- Prevent hypertrophic scar formation.
- Restore function and correct cosmetic defect.
- Prevent recurrence of injury and promote accident prevention.
Age
The younger the child, the more likely shock will occur for a given extent of burn.
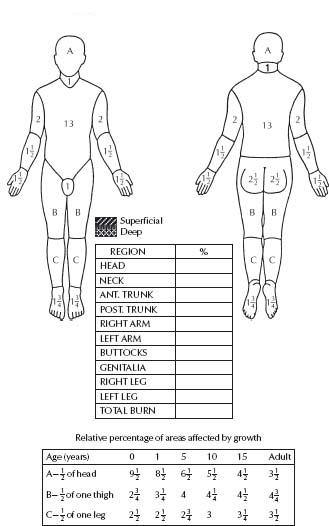
Estimating the surface area burned
The usual adult formula (rule of nines) is not applicable to children. In infancy, the head is relatively large and contributes proportionately more to the total surface area. As the child grows, the lower limbs contribute more to the total surface area. The burned areas should be plotted accurately on the body chart and the area calculated with the aid of the Lund– Browder chart (see Fig. 20.1). The extent of the burn is commonly overestimated, leading to excessive fluid administration.
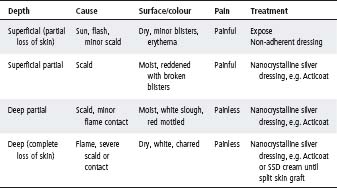
Assessment of the depth of burn
In most burns, there are varying grades of injury (see Table 20.1).
- Remove clothing or smother the flame immediately.
- In minor burns, apply cold water from a bowl or by compressing for up to 30 min.
- In major burns, bathe for 20 min whilst awaiting transportation to hospital. Never use ice or ice slush.
- Cover to guard against hypothermia or cold injury with special foam transport dressing (if available) or plastic cling wrap, with a blanket for warmth. Give i.v. fluid, oxygen and morphine.
- Chemical and eye burns should be irrigated with copious volumes of cold water.
- Check tetanus immunisation status and boost with tetanus toxoid ± tetanus immunoglobulin as appropriate (see chapter 3, Procedures, p. 51).
Table 20.1 Assessment of burn depth
Pain relief
- Paracetamol (oral), 20–30 mg/kg.
- Codeine (oral), 0.5–1 mg/kg.
- Morphine (i.v.), 0.1 mg/kg given in titrated boluses.
- Morphine (i.m.), 0.2 mg/kg (useful if only a single dose is anticipated).
Superficial burns <5% of the body surface area (BSA) are suitable for outpatient treatment, unless they occur on the face, neck, hands, feet or perineum. Infants <12 months are more likely to require admission.
Initial management
- Blisters should be left intact.
- Gently cleanse and remove loose skin.
- If burns are definitely superficial, dress with tulle gras and an absorbent dressing (e.g. gauze). Do not use Hypafix-type dressing directly on the burn.
- Immobilise with a crepe bandage, plaster slab or sling, if indicated.
- In partial thickness burns of indeterminate depth, the use of nanocrystalline dressing is recommended e.g. Acticoat. These dressings should be left in place for 3 or 7 days depending on the product used.
Subsequent management
- Leave the initial dressing for 5–8 days. If the dressing is soaked by exudate, redress without disturbing the adherent tulle.
- If the healing process is not complete by the end of the second week, grafting may be required. Deep, second-degree burns should be grafted by 5–10 days.
- Pain, fever and soiled or offensive dressings indicate that the dressing should be changed and the child assessed and treated for infection if necessary.
Superficial burns >5% of the BSA and deep burns require admission to hospital. For any child with burns >10% of the BSA, consider transfer to a specialist paediatric burns centre. Older children with more extensive superficial burns, such as sunburn, may be managed as outpatients (see Table 20.1).
General
- Document the time, causative agent, circumstances of the burn, therapy initiated and the child’s general health. If the history is inconsistent with the injury, consider child abuse.
- Carefully chart the extent and depth of the burn.
- Weigh the patient if possible.
- In burns >10% of BSA, insert an i.v. line. If a central venous line is needed, a specialist burn centre should be involved. Plan i.v. therapy (see below) and commence treatment with Hartmann’s solution.
- Draw blood for baseline laboratory studies, including haemoglobin, haematocrit and serum electrolytes. In severe burns include blood group and a cross-match.
- In burns >15% of BSA, insert a silastic urethral catheter for hourly urine volume.
- Analgesia or sedation should be administered as necessary (see chapter 4, Pain management).
- Prevent infection. Care should be taken in ward management to guard against cross-infection. Antibiotics should not be prescribed routinely.
- Observations of general condition, pulse, respiration rate, temperature, BP and fluid balance (including hourly urine output estimations) are necessary.
Respiratory management
- With severe burns to the face, consider early endotracheal intubation. As the face swells, airway obstruction may occur, making intubation difficult.
- •Smoke inhalation may lead to acute respiratory distress syndrome (ARDS) where ventilation perfusion defects result in hypoxemia, alveolar collapse, shunting and decreased lung compliance.
- Carboxyhaemoglobin (COHb) and cyanide concentration should be measured in all burn/ smoke inhalation patients. Symptoms of hypoxemia manifest at levels >30% COHb. Treatment is oxygen therapy, as CO binding to Hb is reversible.
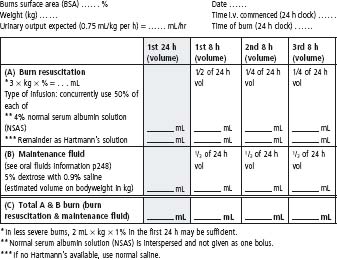
Fluid management
Fluid resuscitation
See Figure 20.2.
- Fluid volume = 3 mL/kg body weight/% burn surface area (BSA) in the first 24 h.
- In less severe burns, fluid volume = 2 mL/kg body weight/% BSA may be sufficient.
- Type of fluid = 4% normal serum albumin solution (NSAS) and Hartmann’s solution (use 50% of each solution concurrently).
Fluid maintenance
- 5% dextrose with 0.9% saline (to calculate maintenance fluid rate see chapter 5, Fluids, p. 73).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree