Case 17 Recurrent wheeze
Caroline, a 2½-year-old girl, was brought to the Paediatric ED by staff at her nursery because she had suddenly developed a cough and a wheeze. They reported that she had been well all day and was playing quite happily with a doll after lunch. In accordance with Caroline’s parents’ instructions, nursery staff had given her 4 puffs of salbutamol via a spacer but she had become very upset and had not improved. When her parents arrived in the ED the ST1 obtained a history of previous viral induced wheeze and treated with salbutamol via a spacer with good effect. The wheeze had initially developed after an episode of bronchiolitis at 7 months of age, for which Caroline had been in hospital for 4 days needing nasogastric feeds and oxygen therapy. There was no history of a recent illness and no other significant medical history. Caroline’s father had a history of asthma treated with regular inhaled steroids. Neither parent smoked in the house although her father did outside.
Which part of this history should have been explored in greater detail?
On examination Caroline looked generally well and was not distressed. Her temperature was 37.1°C, pulse 88/minute, respiratory rate 28/minute with mild intercostal and subcostal recession. On auscultation there was bilateral expiratory wheeze greater on the right than the left. There was also reduced air entry in the right lower zone posteriorly. Percussion was normal throughout. The remainder of the examination was unremarkable. Her height and weight both plotted on the 25th centile which was appropriate for the family.
Would you have requested a CXR at this stage? If so, why?
A diagnosis was made of probable viral induced wheeze and the reduced air entry ascribed to probable mucus plugging and atelectasis. She was given 10 puffs of salbutamol via a spacer and when reviewed by the ST5 an hour later her chest was much improved, although there was still some wheeze and the signs at the right base were unchanged. Caroline was discharged home with advice to continue with regular salbutamol for 48 hours or until better. There was a discussion about the possibility that this was a first episode of asthma and that Caroline might in due course require preventative treatment like her father. This was mentioned in the discharge summary to the GP. Her inhaler technique was assessed as adequate.
What is your view of this management?
Three months later Caroline presents again to the ED with a high fever, cough and a wheeze. The ST2 records that she is toxic and flushed with a temperature of 38.7°C, pulse 110/minute, respiratory rate 36/minute and oxygen saturation 92% in air. Auscultation shows widespread wheeze and reduced air entry and dullness at the right base with some crackles. The GP referral letter comments that this is Caroline’s third episode in six weeks of right sided signs requiring antibiotics and a CXR he requested during the second episode had shown right lower lobe abnormalities. She is given a salbutamol nebulizer and a dose of paracetamol. A second CXR is requested. An hour later she is reviewed by the ST4. Her temperature is 37.4°C and she is playing in the playroom. He notes her fruity cough and confirms the findings of some dullness and crackles in the right base but the wheezing has improved. He interprets the CXR as showing some consolidation in the right lower lobe. The parents are experienced in giving the salbutamol and he concludes that Caroline is well enough to go home with a course of oral amoxicillin. The parents are advised to consult their GP if she is no better in a few days time.
Was this a reasonable plan?
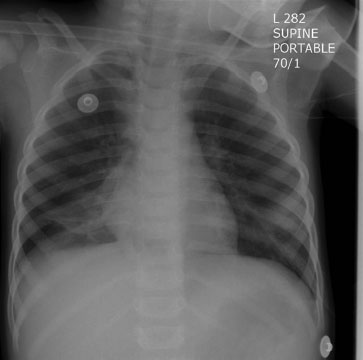
Four months later Caroline is referred by the GP to outpatients because of recurrent episodes of high fever, cough and anorexia with intermittent wheeze. The GP started her on regular inhaled steroids 2 months earlier, but with no improvement. Her inhaler technique has been assessed as good by the asthma nurse in the surgery. On occasions there has been reduced air entry and crackles at the right base and he mentions the changes reported on the CXR he had requested. Caroline has been given several courses of oral antibiotics which do seem to have helped. On examination she is pale but playing quite happily. Her weight has fallen to between the 2nd and 9th centiles but her height is still following the 25th centile. There is dullness to percussion at the right base with reduced air entry and crackles. A CXR shows collapse and consolidation of the right lower lobe (Case Figure 17.1).
< div class='tao-gold-member'>