Definition
The term osteochondroses is used to describe a group of distinct conditions, affecting children between the ages of 2 and 16 years, which involve the growth plates of developing bones. Some of these conditions can severely limit the young athlete.
Key Concepts
Key Concepts
Depending upon the anatomical site and the extent of the condition, effects of the osteochondroses can be either transient or chronic.
Introduction
The child sports participant presents a range of unique issues to the clinician. Some three-quarters of all sports injuries in children have been found to involve the lower limb. The practitioner needs to have good knowledge of developmental biomechanics, sports played and also injury management to be able to diagnose and manage these children effectively.
Children’s unique and susceptible developmental features are outlined below (Brukner & Khan 1993, Frank et al 2007). Each of the following factors play a part:
Osseous growth precedes soft tissue growth
This often results in functional inflexibility and reduced joint ranges of motion until soft tissue elongation occurs. Coordination may be affected as running styles adapt to a changing musculoskeletal frame.
Growth ‘spurts’ increase injury risk
Puberty is associated with twice the usual injury incidence rate. Skeletal growth in parallel with increased sporting participation and intensity can see the young sportsperson side-lined with injury which diminishes both participation and enjoyment.
Apophyses
The apophyses are growth plates (epiphyses) with tendinous attachment which are susceptible to traction forces as muscle–tendon units contract. By definition the apophyses are transient within osseous development, but significant lower limb sites can be a focus of apophyseal inflammation, pain and functional restriction, e.g. tibial tubercle (Osgood–Schlatter’s), calcaneus (Sever’s).
Epiphyseal activity
Like the apophyses, the very existence of these growth centres delineates children’s skeletons from those of adults where the epiphyseal activity has ceased. These regions are more vulnerable to injury and if the growth plate per se is involved, it may retard the final development of that region.
Peer/gender inequality
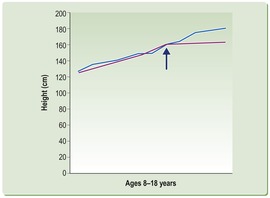
As Figure 13.1 illustrates, females and males develop at different rates and there is also variable development within same gender age groups. Differing body mass and strength can be implicated in injury outcomes, an obvious example being injuries from collision where disparate body masses are involved.
Injury mechanisms
There are basically two types of injuries that occur in children playing sports: macrotrauma or microtrauma. Macrotrauma is usually due to collision in comparison to microtrauma, which is an overuse injury of the child’s body – too much activity and too frequently played.
Stress–strain curve
A strain on a material can be defined by the change in the material’s dimension, and any force acting on a material produces a stress (y). With tensile materials, strain (x) is the same as stretch, and is simply the ratio of the change in size to the original size. Young’s modulus of elasticity (E) is the ratio between stress and strain:


E is the slope of the stress–strain graph: the steeper the slope, the stiffer the material. The maximum height of the stress–strain curve is called the tensile strength, which is a measure of the amount of stress a material can take before tearing apart. The extensibility, or breaking strain, is the furthest horizontal extent of the stress–strain curve and, like strain, it is dimensionless. We can graph Young’s modulus to see how stiffness changes as strain increases.
Young’s modulus of elasticity can be thought of as a measure of how well a substance stands up to tension.
Let us consider the concepts offered by Young’s modulus in relation to the young athlete:
The ligaments in children are relatively stronger than the adjacent bone or cartilage. As a result the young athlete often incurs bone or epiphyseal fracture when the same injury in an adult would produce ligament disruption, e.g. lateral ankle inversion sprain. The child is much more elastic than the adult.
The muscle–tendon unit, which is commonly injured following excessive strain in adults, is usually spared in children, who are more likely to develop pathology at the tendon–bone junction, e.g. Sever’s (calcaneal apophysis) versus Achilles tendon problems. Tendon ruptures are very unusual in the young athlete.
The child’s bony skeleton, like the tendons and ligaments, shows a vast ability to absorb load without major damage. Young bone is more pliable than older more brittle bone. However, young bone will often injure before young soft tissues, especially if bone is loaded repetitively (giving inadequate repair time) or if a huge load is applied (i.e. macrotrauma) (Ch. 3).
Key Points
Key Points
• The child is much more elastic than the adult.
• Tendon ruptures are very unusual in the young athlete.
• Young bone is more pliable than older more brittle bone.
• Young bone will often injure before young soft tissues.
Bone mineral density
Total body calcium advances from 25 grams at birth to 1000 grams by 15–20 years. Low bone mass results in increased fracture risk, with the aetiology of osteoporosis being multifactorial. Fracture risk may be due to the failure to reach peak bone mass (poor nutrition and low physical activity in childhood are common factors) or accelerated bone loss (smoking, alcohol, reduced exercise, poor diet). Both genetic and environmental factors influence bone mass. Maternal hip fracture history doubles the risk of hip fracture in white women (Seeman 1996). Lean body mass, alcohol intake, cigarette smoking, lack of exercise and diet depleted in calcium, phosphorus, vitamins A, B12, C, D are all implicated factors.
Adult influences
The ‘ugly adult who barracks loudly from the sidelines and urges children to ‘win!, win!’ does not realize that their child is unlikely to have winning as their primary concern when they participate in sport. Numerous authors (Brukner & Khan 1993, Frank et al 2007, Gould 1990) have found a mismatching of desired outcomes between children playing sports and the adults around them (parents, coaches, trainers). It has been found that coaches’ and parents’ excessive desire to win (through their children) actually reduces children’s enjoyment of sport and promotes the ‘drop-out’ rate (Brukner & Khan 1993, Dyment 1991).
It is pertinent to look at the reasons children play sport. It has been found that most young athletes are motivated to play because they want to have fun and enjoy the games. Winning is much lower on their priority list. The drop-out rate of children from sport has been found to be very much influenced by the adult’s ‘win, win’ bias. There are enormous implications for the health dollar if children are inadvertently discouraged from sports and physical activity.
Recent data have estimated that on average Australians are gaining weight at a rate greater than 1 gram per day. Overweight, obesity, diabetes, metabolic syndrome and mental illness may all be reduced by maintaining regular exercise and physical fitness. Regular exercise is an important part of developing a healthy lifestyle and it is recommended that young people are physically active for 60 minutes each day (Sports Medicine Australia 2008).
Preventing sports injuries in children: basic principles
Proactive: injury prevention
• Encouraging children to play a range of sports not only reduces injuries from physical overuse but also builds better overall skills.
• Warm up and cool down as part of training and playing are recommended.
• Levels of training need to be age appropriate. Sports Medicine Australia provides Safety Guidelines for Children in Sport (www.sma.org.au; readers should investigate comparable guidelines in their own countries).
• Hydration, weather, diet, sun protection and footwear are all important and changing needs for children playing sport.
• A school or sporting club pre-participation musculoskeletal screening of children is very useful to detect children who are at increased injury risk. Flexibility, posture, biomechanics, motor skills are areas which can be assessed such that children can better avoid potential injuries (www.smartplay.com.au).
Reactive: injury management
• RICER (rest, ice, compression, elevation, referral).
• No HARM (no heat, no alcohol, no running, no massage).
• It is often necessary to reduce training loads by up to 50% in the acute stages. It is important to be aware how distressing this can be for young sports participants and it is beneficial to spend time explaining the costs and benefits. It is often possible for sport to continue if loads are reduced.
• Local measures to accommodate injuries can be effective in maintaining sport participation (e.g. heel raises for Sever’s cases).
• Correcting identified faults is an essential part of injury management, prevention and better ongoing performance. Typically, areas which need to be addressed include:
Muscular imbalances, e.g.:
– hamstrings and quadriceps
– triceps surae and long foot extensors
– peroneals and tibialis posterior.
Faulty biomechanics:
– supinated/cavus feet (prone to ankle inversion injury)
– pronated feet (prone to MTSS, PFS; see page 261).
• Reviewing young athletes is important, especially pre-season. Footwear advice is fundamental to this process as the wrong choice can be problematic in terms of injury and expensive to correct.
Specific lower limb problems
The osteochondroses are an interesting group of conditions which affect the developing skeleton, making active children susceptible.
Key Concepts
Key Concepts
Lower limb osteochondroses are dominated by Osgood–Schlatter’s disease (affecting the knee/tibial tubercle), which is the most common, and Perthes’ (Legg–Calvé–Perthes’) disease (affecting the hip), which is potentially the most consequential.
While often transient (e.g. Sever’s, affecting the heel), the osteochondroses are important as they can prevent or deter children from sport. Subsequent implications, such as reduced physical activity, can be far reaching when we consider the rise of childhood obesity. Although often referred to as ‘diseases’, the osteochondroses are finite conditions and many do not have lasting sequelae (there are notable exceptions in some cases of Perthes’, Freiberg’s and Köhler’s). These conditions are largely specific to children, involving growth plates, which are eliminated with epiphyseal closures (Bloomfield et al 1992, Brukner & Khan 1993, Gould 1990).
The osteochondroses are a group of conditions affecting the growth plates. Although the aetiology of the osteochondroses is not particularly well understood, the non-articular types are associated with overuse. A possible interplay between mechanical and vascular factors may occur, where increased forces may diminish bone blood flow and in turn the less perfused/weaker bone yields more easily to loads.
Classification
An ordered classification is a useful guide for the clinician dealing with any of the osteochondroses (Bloomfield et al 1992). Table 13.1 uses this approach for the conditions to be discussed within this chapter.
| *Each condition can be classified as non-articular, articular or physeal. | ||||
| **Really a Salter–Harris type 1 fracture or epiphysiolysis. | ||||
| Non-articular | Articular | Physeal | ||
|---|---|---|---|---|
| Crushing, subchondral | Splitting, chondral | |||
| Scheuermann’s | x | |||
| Legg-Calvé-Perthes’ | x | |||
| Slipped capital epiphysis** | ||||
| Osgood–Schlatter’s | x | |||
| Sinding–Larsen–Johansson | x | |||
| Sever’s | x | |||
| Iselin’s | x | |||
| Freiberg’s | x | |||
| Köhler’s | x | |||
| Buschke’s | x | |||
| Osteochondritis dissecans | x | |||
The most commonly encountered osteochondroses (lower limb vicinity) are discussed in the following sections. Table 13.2 provides a useful clinical summary.
| MPJ = metatarsophalangeal joint. | ||||||
| While uncommon, the differential diagnosis of a bone tumour must always be included in the clinician’s differential diagnostic work-up. | ||||||
| Age (years) | Structure | Factors | Onset | Differential diagnoses | ||
|---|---|---|---|---|---|---|
| Scheuermann’s | 12–16 | Thoracic spine | Increased thoracic kyphosis and lumbar lordosis Sports: gymnastics Tight hamstrings | a. painful b. non-painful – typical | Scoliosis Disc disease | |
| Legg–Calvé–Perthes’ | 4–10 | Femoral head | More common in boys | Limp, refuse to weight-bear | Femoral head necrosis | |
| Slipped capital epiphysis | 12–16 | Femoral head | More common in boys | Growth spurts | Fracture of physis | |
| Osgood–Schlatter’s | 8–15 | Anterior tibial tubercle | Patella alta Imbalance between hamstrings and quadriceps | Kicking sports Running Jumping | Osteogenic sarcoma | |
| Sinding–Larsen–Johansson | 8–15 | Inferior patella pole | ||||
| Sever’s | 8–15 | Calcaneal apophysis | Tight triceps surae Poor footwear Growth Poor training Pronated foot | Heel pain Limp Worse barefoot Worse in morning Pain with ‘squeeze’ | Brodie’s abscess Osteomyelitis Sero-negative status | |
| Iselin’s | 8–15 | 5th metatarsal styloid process | Poor footwear Growth Pronated foot | Lateral foot pain Limp Shoes aggravate Local tenderness Worse with forefoot abduction | Os vesalianum Peroneus brevis Lateral plantar fascial slip Apophyseal fracture | |
| Freiberg’s | 12–16 | 2nd metatarsal head (or 3rd, 4th) | Foot type Sports Shoes Training | Local tenderness Dorsal prominence Reduced MPJ range | Stress fracture | |
| Köhler’s | 2–8 | Navicular | Spontaneous Pronated foot Pre-coalition | Limp < div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


| ||