Cardiorespiratory arrest
Cardiorespiratory arrest may occur in a wide variety of conditions that cause hypoxaemia or hypotension, or both. Examples include trauma, drowning, septicaemia, sudden infant death syndrome, asthma and congenital anomalies of the heart and lung.
The initial cardiac rhythm discovered during early resuscitation is usually severe bradycardia or asystole. Although the spontaneous onset of ventricular fibrillation in children is approximately 10%, it may occur more frequently with congenital heart conditions or secondary to poisoning with cardioactive drugs. In hospital, respiratory arrest alone is more common than cardiorespiratory arrest.
Diagnosis and initial management
- Cardiorespiratory arrest may be suspected when the patient becomes unresponsive or unconscious, is not moving or breathing normally or appears pale or cyanosed. Call for help.
- Assess airway and respiration by observing movement of the chest, as well as listening and feeling for expired breath while positioning the head and neck to open and maintain an airway. Movement of the chest without expiration indicates a blocked airway.
- Assess circulation by palpation of the carotid, brachial or femoral pulse and by other signs of circulation (adequate breathing, movement, consciousness).
- Whenever possible, manage in a treatment room. Carry the patient there if necessary. If this is not possible, fetch the resuscitation trolley from a treatment room.
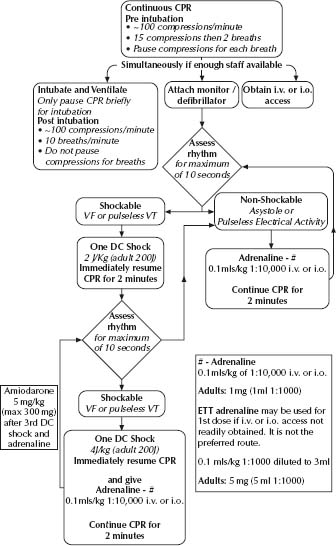
- Cardiopulmonary resuscitation (CPR) must commence with basic techniques and be continued using advanced techniques (Fig. 1.1).
Airway maintenance and ventilation
- If airway obstruction is present, quickly inspect the pharynx. Clear secretions or vomitus by brief suction using a Yankauer sucker.
- Maintain the airway with backward head tilt, chin lift or forward jaw thrust.
- If adequate spontaneous ventilation does not resume, ventilate the lungs mechanically with a self-inflating resuscitator (e.g. Laerdal, Ambu, Air-viva) with added oxygen 8–10 L/ min. If ventilation cannot be achieved with the resuscitator, use a mouth-to-mask technique. Give two initial breaths.
Note: Self-inflating bags (e.g. Laerdal) have a one-way valve and will provide no gas flow to the patient unless they are compressed cyclically.
- Whatever technique is used, ensure that ventilation expands the chest adequately.
- Intubate the trachea via the mouth if possible, but do not cause hypoxaemia by prolonged unsuccessful attempts. Select the tube and insert it at a depth appropriate to the patient’s age in years.
Endotracheal tube (ETT) size and position
- Tube size (internal diameter) = (age/4) + 4 mm (for patients over 1 year of age)
- Depth of insertion is approximately (age/2) + 12 cm from the lower lip Neonates: see Table 32.1 p435
Secure the tube with cotton tape around the neck or affix it firmly to the face with adhesive tape to avoid endobronchial intubation or accidental extubation.
External cardiac compression
Start external cardiac compression (ECC) over the lower sternum if:
- A pulse is not palpable within 10 s.
- A pulse is less than:
– 60 beats/min (for infants)
– 40 beats/min (for older children).
- Other signs of circulation (adequate ventilation, movement, consciousness) are absent.
Place the patient on a firm surface and depress the lower sternum one third the depth of the chest:
- Newborn infant or an infant (<1 year) – two-thumb technique in which the hands encircle the chest.
- Small child (1–8 years) – the heel of one hand.
- Larger child (>8 years) and adult – the two-handed technique.
Avoid pressure over the ribs and abdominal viscera.
Compression–ventilation rates and ratios
The rates and ratios recommended for healthcare rescuers by the Australian Resuscitation Council (www.resus.org.au) are shown in Table 1.1.
When using bag-to-mask ventilation or mouth-to-mask ventilation, the rescuer giving compressions should count aloud to allow the rescuer giving ventilation to deliver effective breaths during pauses between compressions with minimal interruption in compressions. Compression may be commenced at the end of inspiration.
The rate of compression is 100/min, that is one compression every 0.6 s, aiming to give approximately 80–100 actual compressions each minute.
If ventilation is given by bag and ETT, ECC may be continued during ventilation provided lung expansion can be achieved. In this circumstance, restrict the number of ventilations to about 10/min.
Management of cardiac dysrhythmias
Determine the cardiac rhythm with defibrillator paddles or pads or chest leads.
Table 1.1 Compression–ventilation ratios (from the Australian Resuscitation Council)
| Give 2 initial breaths, then | ||
| One rescuer (expired air resuscitation) Compression : breaths | Two rescuers (bag–mask ventilation) Compression : breaths | |
| Newborn infants | 3:1 | 3:1 |
| Infants (<1 yo) | 30:2 | 15:2 |
| Small children (1–8 yo) | 30:2 | 15:2 |
| Larger children (>8 yo) | 30:2 | 15:2 |
| Adults | 30:2 | 30:2 |
- Give DC shock if ventricular fibrillation or pulseless ventricular tachycardia is present. See Table 1.2 and Fig. 1.1 for energy doses in DC shock.
- Give adrenaline if any other pulseless rhythm is present (see Fig. 1.1). The dose is: – i.v. and intraosseous: 10 mcg/kg (0.01 mL of 1 : 1000 solution)
– endotracheal tube (ETT): 100 mcg/kg (0.1 mL of 1 : 1000 solution)
- Insert an i.v. cannula. Although this is the preferred access to the circulation, do not waste time (>90 s) with repeated unsuccessful attempts, as access can be achieved with the alternative techniques of:
– Intraosseus administration (see Procedures, chapter 3, p. 39): all i.v. drugs and resuscitation fluids can be given.
– ETT administration: only adrenaline, atropine and lignocaine (lidocaine) can be given; this is the least effective method, with some evidence suggesting possible adverse effects on the circulation.
Other drugs
Calcium
This is a useful inotropic and vasopressor agent but it has no place in the management of a dysrhythmia, unless it is caused by hypocalcaemia, hyperkalaemia or calcium channel blocker toxicity. It is not useful and probably harmful for asystole, ventricular fibrillation or electromechanical dissociation. The i.v. dose is 10% calcium chloride (0.2 mL/kg) or 10% calcium gluconate (0.7 mL/kg). Do not administer calcium via ETT and do not mix it with bicarbonate.
Adenosine
This is the preferred drug treatment (200 mcg/kg i.v.) for supraventricular tachycardia (SVT). See management of SVT in Cardiac conditions, chapter 21, p. 256.
Table 1.2 Table of drugs, fluid volume, endotracheal tubes and direct current shock for paediatric resuscitation
Source: Oakley, P., Phillips, B., Molyneaux, E. & Mackway–Jones, K. (1993) Updated standard reference chart. BMJ 1993; 306, 1613.
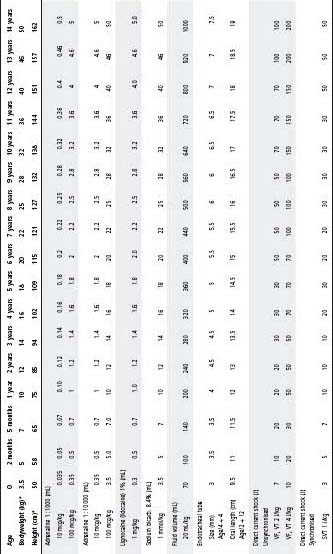
* 50th percentiles.
Post-resuscitation care
- Ensure adequate ventilation and normocarbia.
- Maintain adequate blood pressure with infusion of fluids and inotropic support as needed.
- Do not actively rewarm and if unconsciousness remains after resuscitation, cool to 33– 34 °C within 6 h for 2–3 days.
See also Allergy and immunology, chapter 19.
The life-threatening clinical manifestations are:
- Hypotension due to vasodilatation and loss of plasma volume due to increased capillary permeability.
- Bronchospasm.
- Upper airways obstruction due to laryngeal or pharyngeal oedema.
Immediate treatment
- Vasopressor and bronchodilator therapy: give adrenaline 10 mcg/kg (0.01 mg/kg) at 0.01 mL/kg of 1 : 1000 solution by intramuscular (i.m.) injection or 0.01 mg/kg (i.e. 0.1 mL/kg of 1 : 10 000 solution) by slow i.v. injection (over 10 min). A continuous infusion (0.1–1.0 mcg/kg per min) may be required if manifestations are prolonged. Note: Do not use subcutaneous adrenaline, as absorption is less reliable.
- Oxygen by mask: mechanical ventilation may be required.
- I.v. volume expander: give 0.9% saline at 20 mL/kg. Give repeat boluses of 10–20 mL/kg until the blood pressure is restored.
- Bronchodilator therapy with salbutamol: continuous nebulised (0.5%) or i.v. 5 mcg/kg per min for 1 h, then 1 mcg/kg per min thereafter. Secondary therapy with a steroid, aminophylline and an antihistamine may be helpful for prolonged bronchospasm and capillary leak.
- Relief of upper airway obstruction: mild to moderate oedema may respond to inhalation of nebulised 1% adrenaline (1 mL per dose diluted to 4 mL) or 5 mL of nebulised 1 : 1000 solution, but intubation of the trachea may be required.
- Anaphylaxis can be biphasic and the patient may deteriorate again over the next few hours.
- All patients with anaphylaxis should be observed carefully for at least 12 h, followed up for allergen testing, provided with self-injectable adrenaline and a Medi-alert bracelet.
Allergic oedema causing acute larygeal obstruction
Treat with nebulised 1% adrenaline 1 mL per dose diluted to 4 mL, or 5 mL of 1 : 1000 solution. Refer to an intensive care specialist or anaesthetist for endotracheal intubation, or an ENT surgeon for tracheostomy.
The normal circulating blood volume is 70–80 mL/kg. A child may lose a substantial volume of blood without developing hypotension. Cardiac output and blood pressure are preserved by tachycardia and vasoconstriction, so hypotension is a late sign of blood loss.
- Control external haemorrhage by direct wound pressure, arterial vessel pressure or a tourniquet and elevation of the injured area.
- Administer oxygen by mask.
- Insert a large-bore i.v. cannula, preferably in the upper limb. Two cannulae are usually required.
- Withdraw blood for group and cross-match.
- Infuse rapidly by pressure 20 mL/kg of 0.9% saline solution. This may also be administered rapidly by syringing with the aid of a three-way tap. Titrate additional volume to the heart rate, blood pressure and other indices of perfusion. Further boluses of 10–20 mL/kg 0.9% saline solution may be given.
- If exsanguinating, transfuse urgently with (in order of preference):
– crossmatched blood, or
– un-crossmatched blood of the same group as the patient, or
– un-crossmatched O-negative blood.
- Warm the blood.
- Monitor blood pressure, heart rate, oxygenation and urine output.
- Measure the central venous pressure, serum calcium, serum potassium, coagulation and acid–base status if a massive transfusion is required. Calcium (10% calcium chloride 0.2 mL/kg) and fresh frozen plasma are usually needed after 1–2 blood volumes have been transfused.
- Investigate and surgically explore internal haemorrhage if necessary.
Hypotension is due to vasodilatation, (early) leakage of fluid from capillary beds and depression of myocardial contractility.
- Collect blood for culture, but do not delay administration of an antibiotic if a blood sample cannot be collected. If no information is available regarding the source of pathogen, give flucloxacillin 50 mg/kg (max 2 g) i.v. 4 hourly and cefotaxime 50 mg/kg (max 2 g) i.v. 6 hourly. For particular circumstances consult the Antimicrobial guidelines. For shock due to meningococcaemia, which is usually accompanied by a purpuric rash, give cefotaxime 50 mg/kg (max 2 g) i.v. 6 hourly. Give benzylpenicillin 60 mg/kg (max 3 g) i. v. / i.m. 4 hourly if cefotaxime not available.
- Treat shock with 0.9% saline solution, 20 mL/kg initially – further boluses of 10–20 mL/ kg may be needed.
- Give oxygen and monitor blood gases. Mechanical ventilation may be required.
- Commence infusion of an inotropic agent. Dopamine (5–20 mcg/kg per min) is preferred. Administration via a central vein is preferred but it may be given via a peripheral vein as a dilute solution (e.g. 15 mg/kg in 500 mL at 10–40 mL/h = 5–20 mcg/kg per min). Dobutamine (5–20 mcg/kg per min) may be administered into a peripheral vein.
- Defer lumbar puncture, if indicated, until the child has been stabilised.
There is a global hypoxic–ischaemic injury often associated with lung damage from aspiration of water and gastric contents. The differences between freshwater and saltwater drowning are not usually clinically important.
- Adequate oxygenation and ventilation are of paramount importance. Mechanical ventilation is required for severe lung involvement, circulatory arrest or loss of consciousness. Lung hypoxic–ischaemic injury is compounded by pulmonary oedema or aspiration of water or gastric contents.
- Decompress the stomach, which is usually distended with air and water.
- Support the circulation with i.v. infusion of colloid (e.g. 4% albumin) or 0.9% saline solution and infusion of an inotropic agent (e.g. dopamine 5–20 mcg/kg per min into a central vein).
- If signs of cerebral oedema are present (i.e. a depressed conscious state) administer mannitol 0.25–0.5 g/kg i.v. once.
- Correct electrolyte disturbances; hypokalaemia is common.
- Administer benzylpenicillin 60 mg/kg (max 3 g) i.v. 6 hourly if ventilation is required (to prevent the complication of pneumococcal pneumonia).
- If CPR is required, prevent hyperthermia and induce controlled hypothermia (33–34 °C) for 72 h for cerebral protection.
The most common cause is laryngotracheobronchitis (croup) and occasional causes are epiglottitis, an inhaled foreign body, allergic oedema and trauma. The hallmark of obstruction is stridor, which when accompanied by a barking cough suggests croup, or when accompanied by dysphagia/drooling suggests epiglottitis. Severe obstruction stimulates forceful diaphragmatic contraction that results in a retraction of the rib cage, tracheal tug and abdominal protrusion on inspiration. Cyanosis and irregular respiratory effort are terminal signs.
Epiglottitis
See also Respiratory conditions, chapter 36, p. 513.
- Complete obstruction may occur in just a few hours. In general, tracheal intubation under anaesthesia is required. Arrange promptly.
- Keep the child as calm as possible in a seated position and administer oxygen by mask.
- If complete obstruction is imminent, summon immediate help from an intensivist or anaesthetist. If inexperienced, do not attempt intubation unless the child becomes comatosed. Intubate orally initially with a relatively small endotracheal tube. It may be hard to see the larynx because of secretions in the pharynx and the swollen epiglottis. Be prepared to aspirate the pharynx with a Yankauer sucker. Cricoid pressure is very helpful to visualise the vocal cords.
- If intubation proves to be impossible, attempt to ventilate with bag–valve–mask; a good technique may achieve adequate oxygenation and ventilation. If ventilation is impossible, perform cricothyrotomy or tracheostomy (see below).
- Antibiotic therapy: Ceftriaxone 100 mg/kg (max 2 g) i.v. followed by 50 mg/kg (max 2 g) 24 h later.
Croup
See also Respiratory conditions, chapter 36, p. 515.
- Avoid any examination that may distress the child.
- In severe obstruction, give an inhalation of nebulised 1% adrenaline 1 mL per dose diluted to 4 mL, or 5 mL of 1 : 1000 solution to obtain temporary relief.
- Give corticosteroid i.m/i.v. (e.g. dexamethasone 0.6 mg/kg).
- Obtain intensive care or anaesthetic help with a view to endotracheal intubation. If this is not available, intubate when the child is going into respiratory failure. Use an introducing stylet in an endotracheal tube of size 0.5–1 mm smaller than usually calculated by age in years; i.e. (age/4 + 4 mm).
- Children admitted to a general paediatric ward should not be administered oxygen. Decreased saturations are a marker of obstruction requiring medical review and often further adrenaline. Giving oxygen masks this.
Aspirated foreign body
See also Respiratory conditions, chapter 36, p. 518.
- Give first aid (back slaps, chest thrusts) if obstruction occurs, otherwise allow the child to cough. Do not instrument the airways if the child is coping, but summon an anaesthetist and ENT surgeon. Give oxygen.
- If complete obstruction occurs, attempt removal of an impacted laryngeal foreign body with forceps – if this is unsuccessful, perform cricothyrotomy or tracheostomy (see below).
- If respiratory failure is due to a foreign body lodged in the lower trachea or bronchi, attempt ventilation via an endotracheal tube while organising endoscopic removal.
Emergency relief of a totally obstructed upper airway
- Adequate oxygenation (but not normal ventilation) can be obtained by inserting a 14-gauge i.v. cannula percutaneously into the trachea via the cricothyroid membrane (which lies between the thyroid and cricoid cartilage); the patient should be lying straight, with the cannula in the midline and angled towards the feet. Remove the needle of the i.v. cannula; connect the cannula to a resuscitator or a bagging circuit using a connector from a 3.0 mm endotracheal tube. Oxygenate with sustained 100% oxygen inspirations. Alternatively, connect the cannula to the compressed wall oxygen supply via a three-way i.v. tap (to allow expiration) and a length of plastic tubing. A length of plastic tubing that has a side hole cut may also be used to allow expiration. Aid intermittent expiration by lateral chest compression.
- Alternatively, perform cricothyrotomy. Identify and maintain stabilisation of the thyroid– cricoid region with one hand. Incise the skin over the cricothyroid membrane. Bluntly dissect into the trachea with forceps in the midline or incise vertically with scalpel. Insert a small tracheostomy or endotracheal tube.
- Alternatively, perform percutaneous mini-tracheostomy.
See also Respiratory conditions, chapter 33.
Critical asthma
Children unresponsive to intermittent inhalation of salbutamol should receive:
- Continuous inhalation of undiluted 0.5% salbutamol solution nebulised with oxygen.
- Methylprednisolone 1 mg/kg i.v. (max 50 mg) 6 hourly.
- Nebulised ipratropium may be added as 250 mcg/dose diluted to 2–3 mL every 20 min × 3 and then 4–6 hourly (beware anticholinergic effects).
- I.v. salbutamol load 5 mcg/kg per min for 60 min followed by infusion 1–2 mcg/kg per min (beware hypokalaemia). Discuss with nearest paediatric ICU or retrieval service at this stage.
- Aminophylline (subject to prior theophylline use and serum level) 10 mg/kg (max. 500 mg) i.v. over 1 h. This can be followed by an infusion: 1.1 mg/kg per hour (age 1–9 years) or 0.7 mg/kg per hour (10 years to adult) or 6 hourly doses (each over an hour). Check level following loading dose.
- MgSO4 0.1 mmol/kg infused over 30 min.
- Refractory critical asthma – manage in ICU.
See also Neurologic conditions, chapter 33, p. 453.
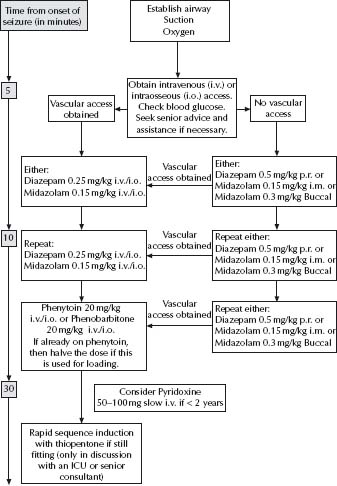
A convulsion involving the respiratory musculature and upper airways that does not cease within a few minutes may cause hypoventilation with hypoxaemia and hypercarbia. Refer to Fig. 1.2 for proposed algorithm on acute seizure management.
- Administer oxygen.
- Be prepared to give mechanical ventilation, particularly if the child has meningitis.
- Check blood glucose, electrolytes, blood gas and septic screen.
- Some initial i.v. anticonvulsant choices include:
– Diazepam: 0.2–0.4 mg/kg (max 10–20 mg) i.v. May be given per rectum if there is no i.v. access.
– Midazolam: 0.1–0.15 mg/kg i.v. or 0.15–0.2 mg/kg (i.m.) effective i.m. within 5–10 min.
– Clonazepam: 0.25 mg (<1 year); 0.5 mg (1–5 years); 1 mg (>5 years) i.v.
– Phenobarbitone: 20–30 mg/kg over 30 min; repeat doses 10–15 mg/kg every 15– 30 min up to 100 mg/kg in 24 h (beware of hypotension) if required (adults – max 600 mg/d).
– Phenytoin: 15–20 mg/kg (max 1.5 g) i.v. over 1 h to avoid negative inotropic effect. Slow onset. Infuse under ECG monitoring.
– Thiopentone: titrate dose slowly to effect (usually 2–5 mg/kg). Beware of hypotension and be ready to control the airway and breathing before administration. This is usually undertaken with ICU support.
- Consider i.v. ceftriaxone if meningitis suspected.
Prolonged convulsions may require large and repeated doses of anticonvulsant drugs or infusions and, consequently, mechanical ventilation. Repeated doses of a single anticonvulsant such as phenobarbitone (where the serum level correlates with the effects) are preferable to using multiple anticonvulsants. Suspect hyponatraemia as the cause of convulsions in meningitis and severe gastroenteritis-related dehydration.
Fig. 1.2 Acute seizure management. (From NSW Heath Acute Paediatrics Clinical Practice Guidelines.) Reproduced with permission, NSW Department of Health from its publication Acute management of seizures in children (December 2004).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree