Case 1 A boy with a limp
Sam, an 11-year-old boy presents to the ED with a limp. He was playing football 2 days earlier but does not recall any injury. He is otherwise well with no history of recent illness. On examination Sam is noted to be obese with a weight of 74 kg. He is apyrexial. He has an obvious limp and Dr Butler, the FY2 in the ED, notes that the movements of the left hip are limited and painful. He does a FBC, CRP and ESR, which are all normal, and orders a pelvic X-ray on which he can see no abnormality. Dr Butler diagnoses a sprained muscle or a transient synovitis and prescribes ibuprofen. He also makes a referral to the paediatric clinic because of Sam’s obesity.
Do you agree with the diagnosis? Would you have managed the case differently?
Sam does not attend that appointment, which is 7 weeks later and is referred back to his GP. Sam sees his GP 3 months after the initial visit to the ED because he still has a limp and the pain has got significantly worse. The GP is concerned about the length of time that the limp has lasted for and refers him to the paediatric rapid referral clinic where he is seen the next day.
In the paediatric clinic he is apyrexial and is noted to have a limp and a leg that is flexed and externally rotated. There is left hip tenderness and a significantly restricted range of movements. There are no other signs. The paediatrician, who also asks about the obesity, discovers that there is a family history of hypothyroidism and that Sam also has a small goitre and is short with a height of 130 cm which is on the second centile.
What investigations would you perform?
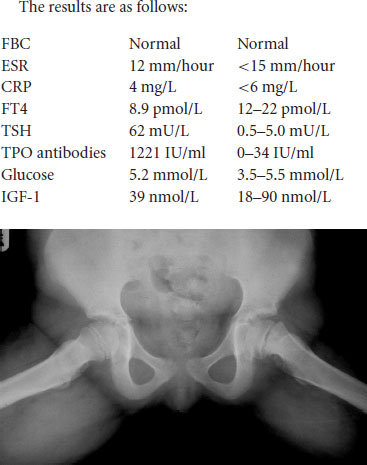
A FBC, CRP, ESR, TFT, TPO antibodies, glucose and an insulin like growth factor 1 (IGF-1) are done and a pelvic X-ray and a frog leg view (see Case Figure 1.1) are obtained.
The paediatrician asks the radiologist to report the X-rays urgently. The radiologist diagnoses a left sided slipped upper femoral epiphysis (SUFE) which is clear on the pelvic X-ray and frog leg views. The radiologist also comments that the slip could be seen on the initial pelvic X-ray 3 months earlier. However, due to an error the initial X-ray was never reported.
What would you do now?
Sam is referred to the orthopaedic team who see him later that day and operate on him the next day pinning the femoral head to the femoral neck. The paediatrician also diagnoses Hashimoto’s (autoimmune) thyroiditis and commences thyroxine.
Following surgery Sam continues to have hip pain, diminished hip movements and a limp and subsequently requires an arthrodesis (hip fusion).
Sam’s mother complains and then sues the hospital, stating that if the diagnosis had been made at the first visit then her son would have not have suffered for so long and would not have required a second operation.
 Expert opinion
Expert opinion
A limp is a common problem in children and requires an evaluation of the back, hip, knee, ankle and foot. The problem may be orthopaedic, rheumatological, neurological or dermatological. One should also remember that hip pain can be referred to the knee. Though it is very important to rule out an infective condition such as a septic arthritis, other conditions must also be considered especially in a child who is systemically well and apyrexial.
SUFE is the most common hip disorder in adolescence. It occurs in children aged 10–16 years with a mean age of 13 years in boys and 11.5 years in girls. It is commoner in boys (2.5:1), on the left and obesity is a risk factor.
Dr Butler, the FY2, should have told Sam’s mother to return to the ED if the pain had not improved within a few days. He should also have known more about SUFE, been aware of the frequency of this disorder in this age group and of the increased likelihood of a SUFE in an obese patient. A FY2 will have little experience in interpreting pelvic X-rays and Dr Butler should have asked an orthopaedic surgeon or radiologist for a second opinion on the X-ray.
In the 10–16 years age group a frog leg (or lateral hip) view is required as some slips are not obvious on the pelvic X-ray. In confirmed cases urgent orthopaedic assessment and treatment are required as even in those with a long history of several months, an acute on chronic slip can occur which can lead to avascular necrosis of the femoral head.
25% of patients also have a contralateral slip and the other hip must therefore be carefully assessed.
A minority of patients with SUFE have an underlying endocrinopathy or metabolic disorder (hypothyroidism, hypogonadism, growth hormone abnormalities, panhypopituitarism or renal osteodystrophy) and if this is suspected then the appropriate investigations should be performed. Obese individuals, such as Sam, should also have their fasting glucose measured. A better history and examination may have led to the diagnosis of hypothyroidism at the initial visit.
Sam’s mother is justified in claiming that the diagnosis of a SUFE should have been made following the initial visit to the ED.
 Legal comment
Legal comment
The expert comment above states that Sam’s mother is justified in claiming that the diagnosis should have been made earlier. An instructed expert is likely to be critical of the actions of the FY2 in ED. Although Dr Butler examined the X-ray he failed to detect the abnormality and did not request a second opinion. The radiologist looking at the X-ray 3 months later commented that the slip was visible on the initial X-ray. Maybe a frog leg or lateral view of the hip should have been taken, as this would have revealed the problem more clearly. Dr Butler also failed to advise Sam’s mother to bring him back if there was no improvement. Earlier intervention may not have cured the problem. However, an instructed expert is likely to conclude that earlier intervention would have made a difference. Thus the case will probably be settled. The claim will be worth at least £70,000 and possibly much more depending on the patient’s prognosis post arthrodesis.