Chapter 51 Elevated or Depressed White Blood Cell Count
ETIOLOGY
How Do White Blood Cells Vary with Age?
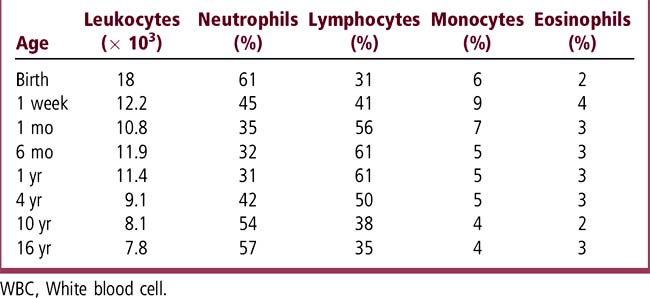
At birth, an infant’s WBC count is high and the differential shows a predominance of neutrophils. This neutrophilic predominance is brief, and by 1 month of age the lymphocytes predominate. The WBC count and differential pattern become similar to that of an adult during early adolescence (Table 51-1). Both leukocytosis and leukopenia can indicate infectious, immunologic, or malignant processes (see Chapter 63 for leukemia).
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree