CARDIOVASCULAR SYSTEM
What is the most likely diagnosis?
a. Aortic dissection
b. Abdominal aortic aneurysm (AAA)
c. Small bowel obstruction (SBO)
d. Renal artery stenosis
Answer b. Abdominal aortic aneurysm (AAA)
An AAA is the most likely diagnosis and presents in a patient older than 65 years of age with a history of smoking and atherosclerotic disease. The findings of an unruptured AAA include periumbilical bruits and a pulsatile mass that is palpable over the abdomen. Aortic dissection causes abdominal disease in patients with a history of hypertension. SBO presents with increasing abdominal girth caused by distension but would be acute (not over the course of a year), and renal artery stenosis does give a bruit but would have elevated blood pressures.
In acute rupture of an AAA, signs and symptoms include abdominal pain, back pain, tachycardia, and unequal blood pressures between the upper and lower extremities.
The U.S. Preventive Services Task Force recommends one-time screening for AAA by ultrasonography in men ages 65 to 75 years who have ever smoked.
What is the biggest risk factor for AAA?
a. Atherosclerosis
b. Hypertension
c. Syphilis
d. Smoking
Answer a. Atherosclerosis
The biggest risk factors for abdominal aortic aneurysm are atherosclerosis and being older than 65 years of age. Hypertension is actually a risk factor for the development of aortic dissection. Syphilis causes aortitis in the thoracic segment of the aorta and attacks the vasa vasorum. Smoking is a risk factor but does not convey the same risk as atherosclerosis.
AAAs are caused by a failure in structural proteins of the aorta, elastin, and collagen combined with overexpression of metalloproteinases, causing remodeling of tissue matrices.
Treponema pallidum causes aortitis through attack on the vasa vasorum or the vessels of the vessels.
What is the best next step in the management of this patient?
a. Ultrasonography
b. Abdominal radiography
c. Computed tomography (CT) scan of the abdomen
d. Magnetic resonance imaging (MRI) of the abdomen
e. Angiography
Ultrasonography is the least invasive and most cost-effective method to obtain management changing information regarding an AAA. Size in a stable unruptured AAA will delineate whether or not the patient will require surgery. Abdominal radiography has very low sensitivity and will only show an AAA if there are calcifications. CT or MRI of the abdomen will offer more information including rostral-caudal extent and if there is extension into the suprarenal aorta. Angiography offers the same information but is overly invasive.
Less frequent causes of AAA include Marfan’s syndrome, Ehler-Danlos syndrome, and collagen vascular diseases.
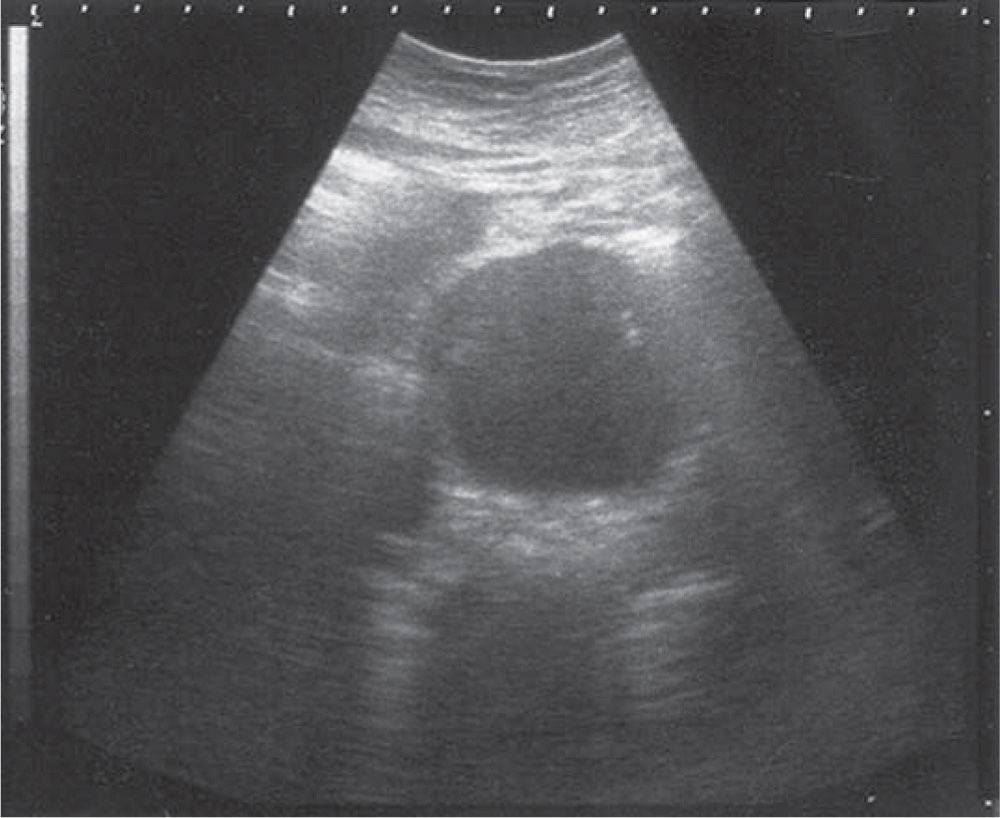
Figure 12-1. Ultrasound image of an abdominal aortic aneurysm in the transverse plane. (Reproduced, with permission, from Tintinalli JE, Stapczynski J, Ma O, et al, eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th ed. New York: McGraw-Hill; 2011.)
What is the best next step in the management of this patient?
a. Observation and repeat ultrasonography in 6 months
b. Observation and repeat ultrasonography in 12 months
c. Surgery after ultrasonography in 12 months
d. Surgery now
Answer d. Surgery now
The patient should have surgery now. AAAs that are larger than 4.5 cm should be referred for surgical intervention because the risk of rupture increases with every centimeter they increase. Observation and ultrasonography is for AAA that are between 3.0 cm and 4.4 cm.
AAAs <3 cm: no follow-up.
AAAs 3 to 4 cm: ultrasonography every 12 months
AAAs 4 to 4.5 cm: ultrasonography every 6 months
AAAs >4.5 cm: surgery
What is the most likely diagnosis?
a. Aortic dissection
b. Abdominal aortic aneurysm (AAA)
c. Pancreatitis
d. Renal artery stenosis
Answer a. Aortic dissection
Aortic dissection occurs when a tear in the intima causes blood to flow between the layers of the wall of the aorta, creating a false lumen. An acute aortic dissection presents with severe chest pain that radiates to the back in the setting of uncontrolled hypertension. Physical examination findings seen in acute dissection are a holosystolic murmur, which is mitral regurgitation; bounding pulses; and interarm arm blood pressure difference of greater than 20 mm. AAAs can present with back pain, but they do not have uncontrolled hypertension, and there would have to be mention of a palpable cystic mass with or without a bruit. Pancreatitis would present with severe epigastric pain and radiation the back; however, this patient presents with severe chest pain. Uncontrolled hypertension does fit the presentation of renal arteries gnosis, but flank pain does not. The flank pain is caused by the dissection crossing the point at which the renal arteries branch from the aorta.
The aorta is composed of the intima, media, and adventitia.
• The intima, the innermost layer, is lined by endothelium.
• The media is responsible for imparting strength and is made of intertwining sheets of elastic tissue.
• The outermost layer of the aorta is adventitia and largely consists of collagen.
• The vasa vasorum, which supplies blood to the outer half of the aortic wall, lies within the adventitia.
Aortic dissections carry a very high mortality rate: one third of patients die within the first 24 hours, and 50% die within 48 hours.
What is the biggest risk factor for the development of aortic dissection?
a. Smoking
b. Hypertension
c. Alcohol use
d. Hyperlipidemia
e. Syphilis
Answer b. Hypertension
Hypertension is the most important factor for the development of acute aortic dissection. In up to 70% of cases, the patients will have uncontrolled blood pressure. Smoking and alcohol use contribute to the development of elevated blood pressure but are not directly linked to the development of aortic dissection. Hyperlipidemia is the correct answer to the question, “Which of the following is most important factor for the development of AAAs?” Syphilis does raise the risk of dissections by involving the vasa vasorum but not as uncontrolled arterial hypertension.
There are only three holosystolic murmurs:
• Mitral regurgitation
• Tricuspid regurgitation
• Ventricular septal defect
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


