a. Increased levels of factors V and VIII
b. A decreased prothrombin level
c. An increased fibrinogen level
d. The presence of fibrin split products
e. Normal partial thromboplastin time (PTT)
405. A male infant was found to be jaundiced 12 hours after birth. At 36 hours of age, his serum bilirubin was 18 mg/dL, hemoglobin concentration was 12.5 g/dL, and reticulocyte count was 9%. Many nucleated RBCs and some spherocytes were seen in the peripheral blood smear. The differential diagnosis should include which of the following?
a. Pyruvate kinase deficiency
b. Hereditary spherocytosis
c. Sickle-cell anemia
d. Rh incompatibility
e. Polycythemia
406. On a routine well-child examination, a 1-year-old boy is noted to be pale. He is in the 75th percentile for weight and the 25th percentile for length. Results of physical examination are otherwise normal. His hematocrit is 24%. The answer to which of the following questions is most likely to be helpful in making a diagnosis?
a. What is the child’s usual daily diet?
b. Did the child receive phototherapy for neonatal jaundice?
c. Has anyone in the family received a blood transfusion?
d. Is the child on any medications?
e. What is the pattern and appearance of his bowel movements?
407. A 10-year-old boy is admitted to the hospital because of bleeding. Pertinent laboratory findings include a platelet count of 50,000/μL, prothrombin time (PT) of 15 seconds (control 11.5 seconds), activated partial thromboplastin time (aPTT) of 51 seconds (control 36 seconds), thrombin time (TT) of 13.7 seconds (control 10.5 seconds), and factor VIII level of 14% (normal 38%-178%). Which of the following is the most likely cause of his bleeding?
a. Immune thrombocytopenic purpura (ITP)
b. Vitamin K deficiency
c. Disseminated intravascular coagulation (DIC)
d. Hemophilia A
e. Hemophilia B
408. A 17-year-old adolescent comes to your office seeking help for “heavy” menses. Your review of systems also reveals weekly epistaxis. Her only significant past history includes a tonsillectomy at age 6 after which she required blood transfusion for excessive bleeding. Her family history includes several people who seem to bleed and bruise more easily than others. The patient’s mother required a hysterectomy after child birth for excessive hemorrhage. You order a variety of laboratory tests. The patient has a hemoglobin of 6.5 mg/dL with an MCV of 60%; her platelet count is 350,000/μL. Her von Willebrand antigen and her von Willebrand factor (vWF) activity (ristocetin cofactor activity) are decreased. Her vWF is reported as normal but in decreased amounts. You have been unable to reach her to report the findings, but when she calls about 1 week later, she reports she is having a mild to moderate nosebleed. You initiate therapy with which of the following?
a. Aminocaproic acid (Amicar)
b. vWF concentrate alone
c. vWF with factor VIII
d. Desmopressin (DDAVP)
e. Intravenous immunoglobulin (IVIG)
409. Over the previous 2 to 3 weeks, a very active 13-year-old white boy is noted by his family to have developed deep pains in his leg that awaken him from sleep. The family brings him to your office with a complaint of a swelling over his distal leg, which he attributes to his being kicked while playing soccer about 1 week ago. He has had no fever, headaches, weakness, bruising, or other symptoms. A radiograph of the leg is shown below. Which of the following is the most appropriate next step?

(Courtesy of Susan John, MD.)
a. Reassurance to the family of the benign nature of the condition
b. Bone marrow aspiration
c. Serial blood cultures and initiation intravenous vancomycin
d. Splinting of leg and reduction in activity
e. Bone biopsy
410. An otherwise healthy 17-year-old boy complains of swollen glands in his neck and groin for the past 6 months and an increasing cough over the previous 2 weeks. He also reports some fevers, especially at night, and possibly some weight loss. On examination, you notice that he has nontender cervical, supraclavicular, axillary, and inguinal nodes, no hepatosplenomegaly, and otherwise looks to be fairly healthy. Which of the following would be the appropriate next step?
a. Biopsy of a node
b. CBC and differential
c. Trial of antituberculosis drugs
d. Chest radiograph
e. Cat-scratch titers
411. An otherwise healthy child has on his 1-year-old routine CBC the polymorphonuclear neutrophil shown below. Which of the following is an appropriate next step?
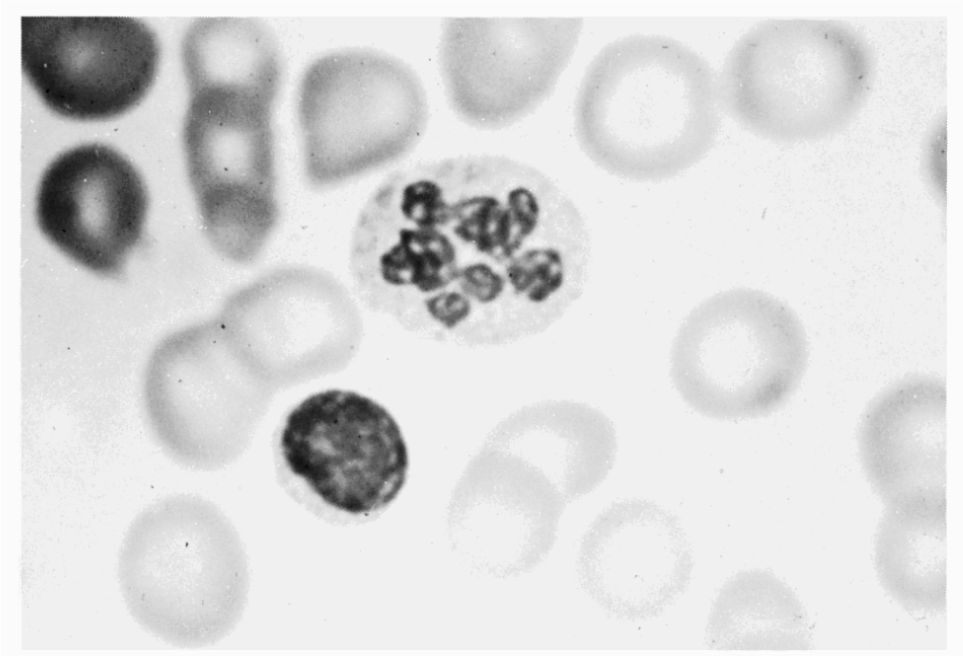
a. Bone marrow aspiration
b. Begin oral iron therapy
c. Begin folic acid supplementation
d. Hemoglobin electrophoresis
e. Initiate monthly infusions of intravenous immunoglobulins (IVIG)
Questions 412 to 415
For each disorder listed below, select the peripheral blood smear with which it is most likely to be associated. Each lettered option may be used once, more than once, or not at all.
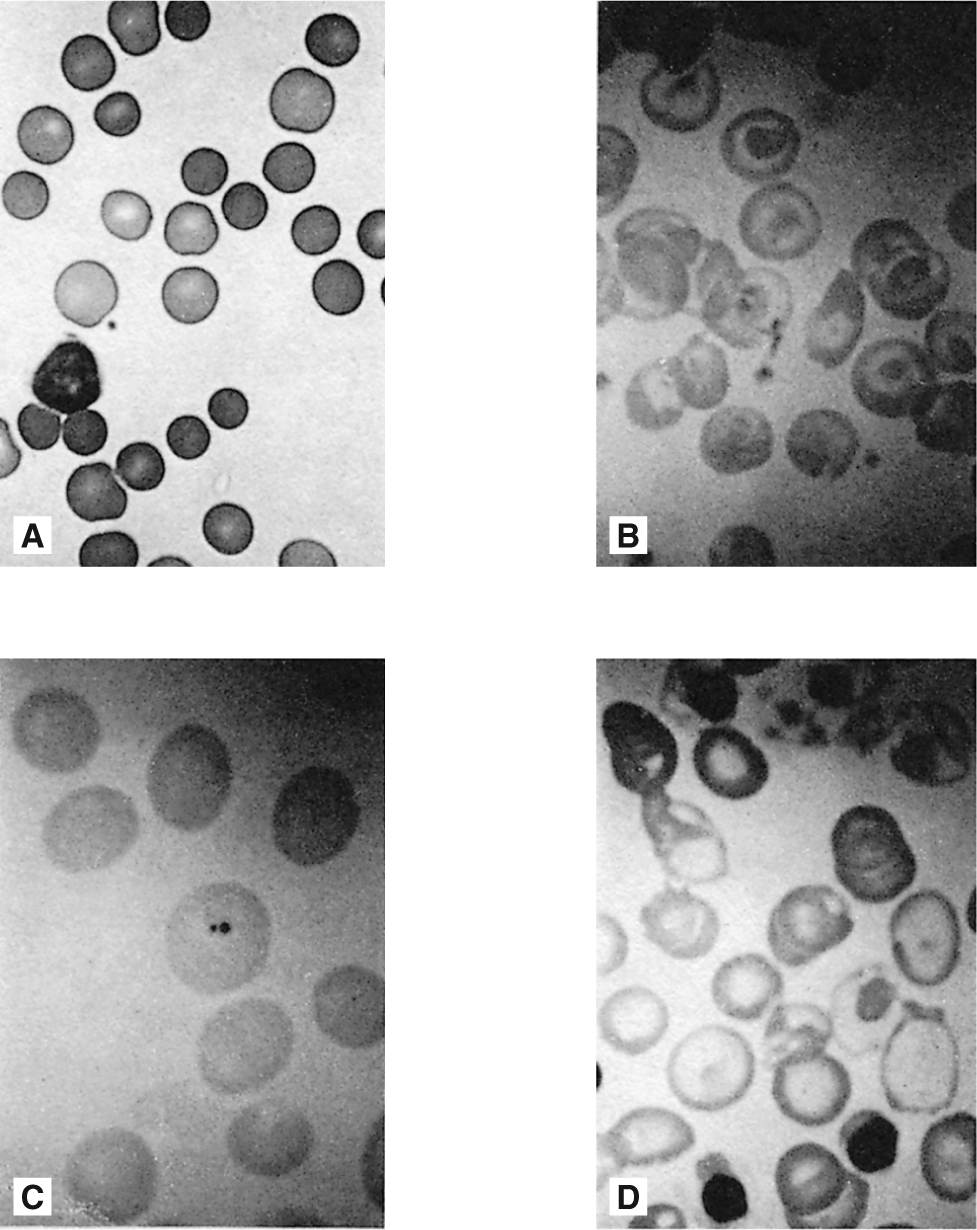
412. An 8-year-old patient has a hemoglobin of 8 mg/dL and repeated hospital admissions for hand pain and swelling.
413. A 9-month-old boy recently moves into your area having been adopted by a family member when his biologic family was unable to care for him. His adoptive family states that they know that he developed progressive anemia over the first months of his life resulting in an admission at about 6 months of age for heart failure and generalized weakness. He has had “a swollen spleen forever” and has had blood transfusions each of the last 3 months.
414. A 2-day-old newborn in the neonatal ICU is receiving phototherapy and has a hemoglobin of 10 mg/dL and a bilirubin of 22 mg/dL.
415. A completely asymptomatic, healthy 1-year-old boy has a hemoglobin of 12 mg/dL. His 35-year-old father states that he has had “mild anemia” his whole life and had a cholecystectomy 2 years ago.
Hematologic and Neoplastic Diseases
Answers
393. The answer is c. (Hay et al, pp 859-861. Kliegman et al, pp 1714-1718. McMillan et al, pp 1731-1733. Rudolph et al, pp 1582-1583.) In children, ITP is the most common form of thrombocytopenic purpura. In most cases, a preceding viral infection can be noted. No diagnostic test identifies this disease; exclusion of the other diseases listed in the question is necessary. In this disease, the platelet count is frequently less than 20,000/μL, but other laboratory tests yield essentially normal results, including the bone marrow aspiration (if done). Complications are uncommon; significant bleeding occurs in only 5% of cases and intracranial hemorrhage is even rarer. The treatment of childhood ITP is controversial. Patients with mild symptoms such as bruising and self-limited epistaxis may be observed, while patients with significant bleeding should be treated. IVIG and corticosteroids are effective in causing a rapid increase in platelet count, but controversy exists surrounding the use of prednisone before ruling out leukemia with a bone marrow aspirate. For Rh-positive patients with a working spleen, the use of anti-D immunoglobulin also results in an increase in platelet count. For patients with chronic (> 1 year) ITP, a splenectomy may be necessary.
Aplastic anemia is unlikely if the other cell lines are normal. vWD might be expected to present with bleeding and not just bruising. It is unlikely that acute leukemia would present with thrombocytopenia only. Thrombotic thrombocytopenic purpura is rare in children.
394. The answer is b. (Hay et al, pp 838-839. Kliegman et al, pp 1655-1658. McMillan et al, pp 1692-1694. Rudolph et al, pp 1546-1548.) Response to a therapeutic trial of iron is an appropriate and cost-effective method of diagnosing iron-deficiency anemia. A prompt reticulocytosis and rise in hemoglobin and hematocrit follow the administration of an oral preparation of ferrous sulfate. Intramuscular iron dextran should be reserved for situations in which compliance cannot be achieved since this treatment is expensive, painful, and no more effective than oral iron. Dietary modifications, such as limiting the intake of cow’s milk and including iron-fortified cereals along with a mixed diet, are appropriate long-term measures, but they will not make enough iron available to replenish iron stores. The gradual onset of iron-deficiency anemia enables a child to adapt to surprisingly low hemoglobin concentrations. Transfusion is rarely indicated unless a child becomes symptomatic or is further compromised by a superimposed infection.
When the iron available for production of hemoglobin is limited, free protoporphyrins accumulate in the blood. Levels of erythrocyte protoporphyrin (EP) are also elevated in lead poisoning. Iron-deficiency anemia can be differentiated from lead intoxication by measuring blood lead, which should be less than 10 μg/dL.
395. The answer is e. (Hay et al, pp 846-848. Kliegman et al, pp 1663-1670. McMillan et al, pp 1707-1709. Rudolph et al, pp 1556-1560
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


