Chapter 332 Acute Gastroenteritis in Children
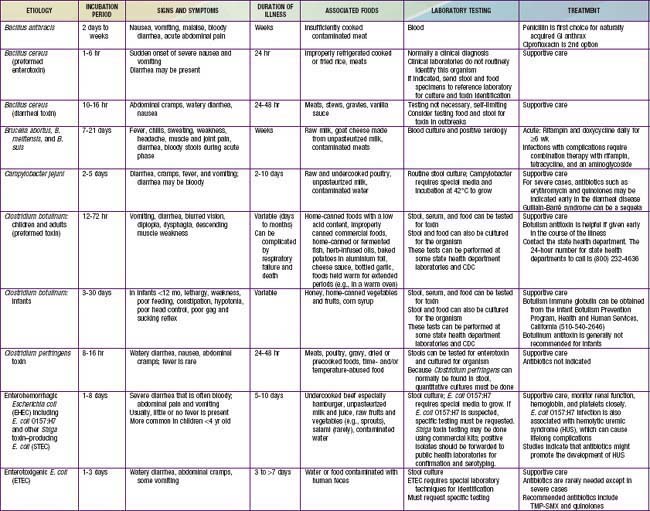
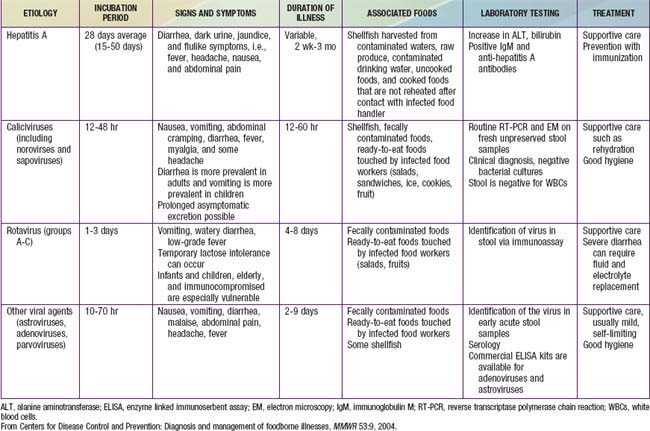
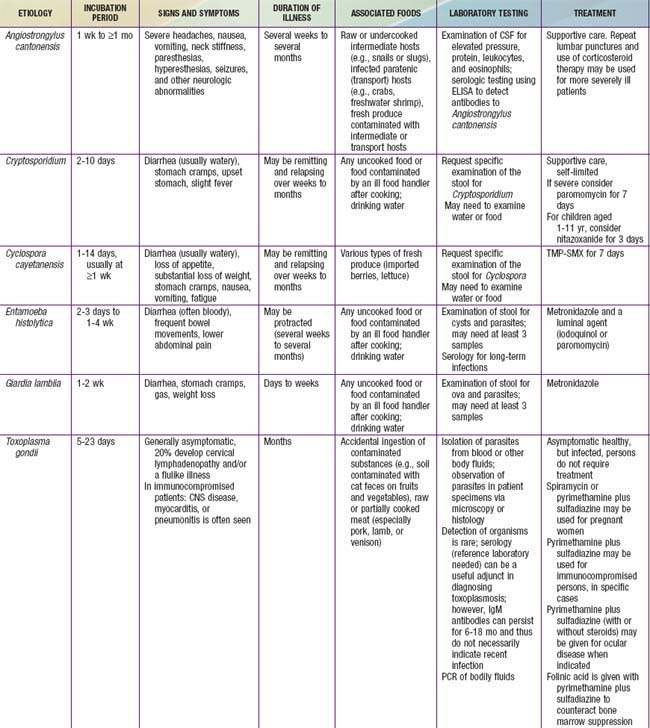
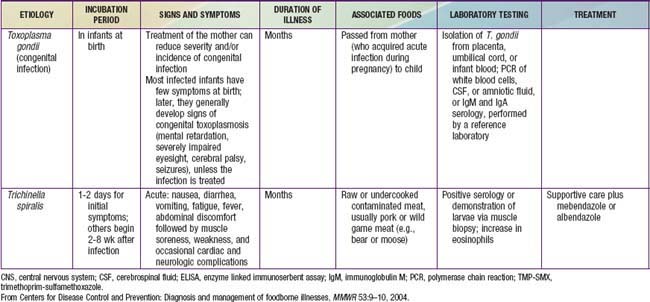
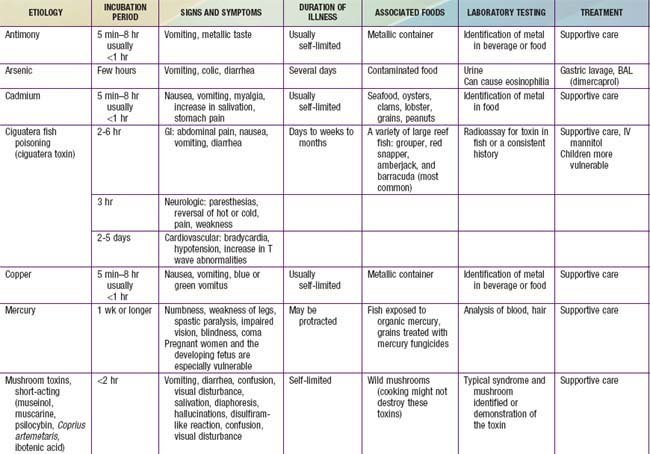
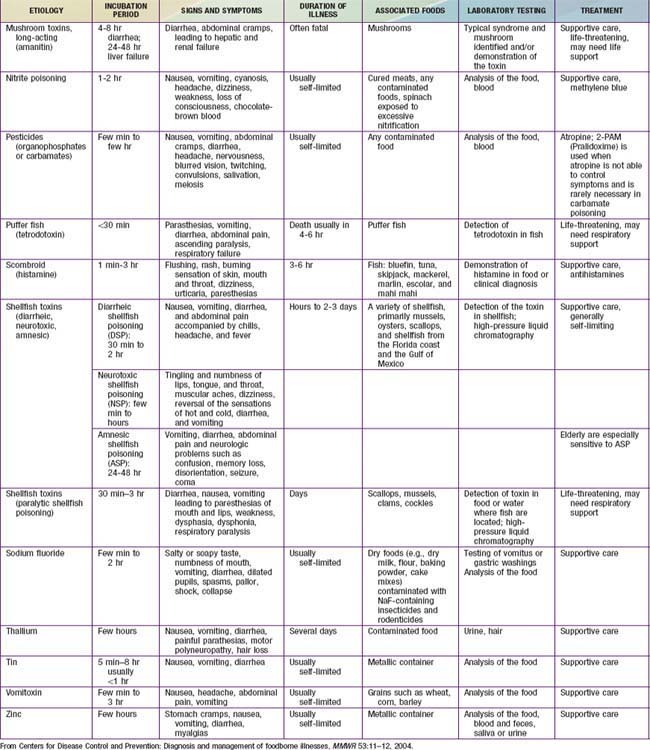
The term gastroenteritis denotes infections of the gastrointestinal (GI) tract caused by bacterial, viral, or parasitic pathogens (Tables 332-1 to 332-3). Many of these infections are foodborne illnesses. The most common manifestations are diarrhea and vomiting, which can also be associated with systemic features such as abdominal pain and fever. The term gastroenteritis captures the bulk of infectious cases of diarrhea. The term diarrheal disorders is more commonly used to denote infectious diarrhea in public health settings, although several noninfectious causes of GI illness with vomiting and/or diarrhea are well recognized (Table 332-4).
Epidemiology of Childhood Diarrhea
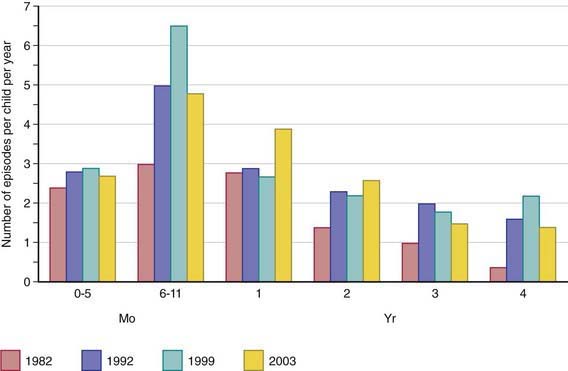
Diarrheal disorders in childhood account for a large proportion (18%) of childhood deaths, with an estimated 1.5 million deaths per year globally, making it the second most common cause of child deaths worldwide. The World Health Organization (WHO) and UNICEF estimate that almost 2.5 billion episodes of diarrhea occur annually in children <5 yr of age in developing countries, with more than 80% of the episodes occurring in Africa and South Asia (46% and 38%, respectively). Global mortality may be declining, but the overall incidence of diarrhea remains unchanged at about 3.6 episodes per child-year (Fig. 332-1), and it is estimated to account for 13% of all childhood disability-adjusted life years (DALYs).
Etiology of Diarrhea
Gastroenteritis is due to infection acquired through the fecal-oral route or by ingestion of contaminated food or water. Gastroenteritis is associated with poverty, poor environmental hygiene, and development indices. Enteropathogens that are infectious in a small inoculum (Shigella, enterohemorrhagic E. coli, Campylobacter jejuni, noroviruses, rotavirus, Giardia lamblia, Cryptosporidium parvum, Entamoeba histolytica) can be transmitted by person-to-person contact, whereas others, such as cholera, are generally a consequence of contamination of food or water supply (see Tables 332-1 to 332-3).
In the United States, rotavirus and the noroviruses (small round viruses such as Norwalk-like virus and caliciviruses) are the most common viral agents, followed by sapovirus, enteric adenoviruses, and astroviruses (see Table 332-2). Food-borne outbreaks of bacterial diarrhea in the United States are most commonly due to Salmonella, E. coli, Clostridium botulinum, Clostridium perfringens, and Staphylococcus aureus followed much less often by Campylobacter, Shigella, Cryptosporidium, Yersinia, Listeria, Vibrio, and Cyclospora species, in that order. Salmonella, Shigella, and, most notably, the various diarrhea-producing E. coli organisms are the most common bacterial pathogens in developing countries (see Table 332-1). Clostridium difficile (by toxin production) is linked to antibiotic-associated diarrhea and pseudomembranous colitis, although most cases of antibiotic-associated diarrhea in children are not due to C. difficile. C. difficile-negative antibiotic-associated hemorrhagic colitis in adults may be due to cytotoxin-producing Klebsiella oxytoca. Waterborne outbreaks are often due to Cryptosporidium species (most common), C. jejuni, noroviruses, Shigella species, Giardia, E. coli O157:H7, Plesiomonas shigelloides, or Vibrio species.
Pathogenesis of Infectious Diarrhea
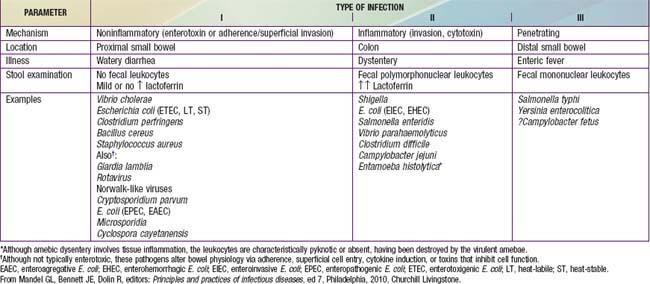
Pathogenesis and severity of bacterial disease depend on whether organisms have preformed toxins (S. aureus, Bacillus cereus), produce secretory (cholera, E. coli, Salmonella, Shigella) or cytotoxic (Shigella, S. aureus, Vibrio parahemolyticus, C. difficile, E. coli, C. jejuni) toxins or are invasive and on whether they replicate in food. Enteropathogens can lead to either an inflammatory or noninflammatory response in the intestinal mucosa (Table 332-5).
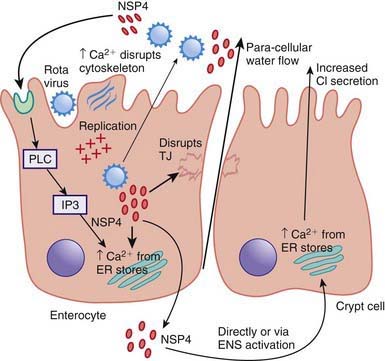
Enteropathogens elicit noninflammatory diarrhea through enterotoxin production by some bacteria, destruction of villus (surface) cells by viruses, adherence by parasites, and adherence and/or translocation by bacteria. Inflammatory diarrhea is usually caused by bacteria that directly invade the intestine or produce cytotoxins with consequent fluid, protein, and cells (erythrocytes, leukocytes) that enter the intestinal lumen. Some enteropathogens possess >1 virulence property. Some viruses, such as rotavirus, target the microvillus tips of the enterocytes and can enter the cells by direct invasion or calcium-dependent endocytosis. This can result in villus shortening and loss of enterocyte absorptive surface through cell shortening and loss of microvilli (Fig. 332-2).
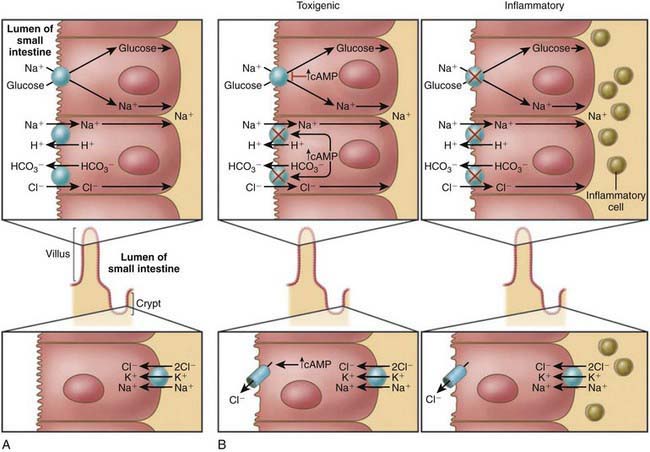
Most bacterial pathogens elaborate enterotoxins; the rotavirus protein NSP4 acts as a viral enterotoxin. Bacterial enterotoxins can selectively activate enterocyte intracellular signal transduction and can also affect cytoskeletal rearrangements with subsequent alterations in the water and electrolyte fluxes across enterocytes. In toxigenic diarrhea enterotoxin produced by Vibrio cholerae, increased mucosal levels of cAMP inhibit electroneutral NaCl absorption but have no effect on glucose-stimulated Na+ absorption. In inflammatory diarrhea (e.g., Shigella spp. or Salmonella spp.) there is extensive histologic damage, resulting in altered cell morphology and reduced glucose-stimulated Na+ and electroneutral NaCl absorption. The role of 1 or more cytokines in this inflammatory response is critical. In secretory cells from crypts, Cl-secretion is minimal in normal subjects and is activated by cyclic adenosine monophosphate (cAMP) in toxigenic and inflammatory diarrhea (Fig. 332-3).
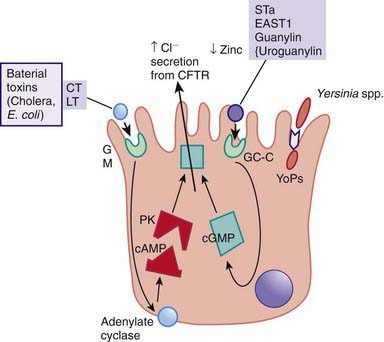
Figure 332-3 Mechanism of cholera toxin.
(Adapted from Thapar M, Sanderson IR: Diarrhoea in children: an interface between developing and developed countries, Lancet 363:641–653, 2004; and Montes M, DuPont HL: Enteritis, enterocolitis and infectious diarrhea syndromes. In Cohen J, Powderly WG, Opal SM, et al, editors: Infections diseases, ed 2, London, 2004, Mosby, pp 31–52.)
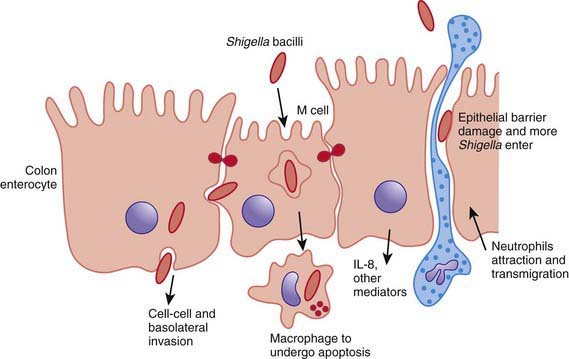
ETEC colonizes and adheres to enterocytes of the small bowel via its surface fimbriae (pili) and induces hypersecretion of fluids and electrolytes into the small intestine through 1 of 2 toxins: the heat-labile enterotoxin (LT) or the heat-stable enterotoxin. LT is structurally similar to the V. cholerae toxin, and activates adenylate cyclase, resulting in an increase in intracellular cyclic guanosine monophosphate (cGMP) (Fig. 332-4). In contrast, Shigella spp. cause gastroenteritis via a superficial invasion of colonic mucosa, which they invade through M cells located over Peyer patches. After phagocytosis, a series of events occurs, including apoptosis of macrophages, multiplication and spread of bacteria into adjacent cells, release of inflammatory mediators (interleukin [IL]-1 and IL-8), transmigration of neutrophils into the lumen of the colon, neutrophil necrosis and degranulation, further breach of the epithelial barrier, and mucosal destruction (Fig. 332-5).
Clinical Manifestation of Diarrhea
Most of the clinical manifestations and clinical syndromes of diarrhea are related to the infecting pathogen and the dose or inoculum (see Tables 332-1 to 332-3). Additional manifestations depend on the development of complications (e.g., dehydration and electrolyte imbalance) and the nature of the infecting pathogen (see Table 332-5). Usually the ingestion of preformed toxins (e.g., those of S. aureus) is associated with the rapid onset of nausea and vomiting within 6 hr, with possible fever, abdominal cramps, and diarrhea within 8-72 hr. Watery diarrhea and abdominal cramps after an 8-16 hr incubation period are associated with enterotoxin-producing C. perfringens and B. cereus. Abdominal cramps and watery diarrhea after a 16-48 hr incubation period can be associated with noroviruses, several enterotoxin-producing bacteria, Cryptosporidium, and Cyclospora and have also been a notable feature of influenza virus H1N1 infections. Several organisms, including Salmonella, Shigella, C. jejuni, Yersinia enterocolitica, enteroinvasive or hemorrhagic (Shigatoxin-producing) E. coli, and V. parahaemolyticus, produce diarrhea that can contain blood as well as fecal leukocytes in association with abdominal cramps, tenesmus, and fever; these features suggest bacterial dysentery and fever (Table 332-6). Bloody diarrhea and abdominal cramps after a 72-120 hr incubation period are associated with infections due to Shigella and also Shigatoxin-producing E. coli, such as E. coli O157:H7. Organisms associated with dysentery or hemorrhagic diarrhea can also cause watery diarrhea alone without fever or that precedes a more complicated course that results in dysentery.
Table 332-6 DIFFERENTIAL DIAGNOSIS OF ACUTE DYSENTERY AND INFLAMMATORY ENTEROCOLITIS
SPECIFIC INFECTIOUS PROCESSES
PROCTITIS
OTHER SYNDROMES
CHRONIC INFLAMMATORY PROCESSES
SYNDROMES WITHOUT KNOWN INFECTIOUS CAUSE
From Mandel GL, Bennett JE, Dolin R, editors: Principles and practices of infectious diseases, ed 7, Philadelphia, 2010, Churchill Livingstone.
Although many of the manifestations of acute gastroenteritis in children are nonspecific, some clinical features can help identify major categories of diarrhea and allow rapid triage for antibiotic or specific dietary therapy (see Tables 332-1 to 332-3). There is considerable overlap in the symptomatology. The positive predictive values for the features of dysentery are very poor; the negative predictability for bacterial pathogens is much better in the absence of signs of dysentery. If warranted and if facilities and resources permit, the etiology can be verified by appropriate laboratory testing.
Complications
Most of the complications associated with gastroenteritis are related to delays in diagnosis and delays in the institution of appropriate therapy. Without early and appropriate rehydration, many children with acute diarrhea would develop dehydration with associated complications (Chapter 54). These can be life-threatening in infants and young children. Inappropriate therapy can lead to prolongation of the diarrheal episodes, with consequent malnutrition and complications such as secondary infections and micronutrient deficiencies (iron, zinc). In developing countries and HIV-infected populations, associated bacteremias are well-recognized complications in malnourished children with diarrhea.
Specific pathogens are associated with extraintestinal manifestations and complications. These are not pathognomonic of the infection, nor do they always occur in close temporal association with the diarrheal episode (Table 332-7).
Table 332-7 EXTRAINTESTINAL MANIFESTATIONS OF ENTERIC INFECTIONS
| MANIFESTATION | ASSOCIATED ENTERIC PATHOGEN(S) | ONSET AND PROGNOSIS |
|---|---|---|
| Focal infections due to systemic spread of bacterial pathogens, including vulvovaginitis, urinary tract infection, endocarditis, osteomyelitis, meningitis, pneumonia, hepatitis, peritonitis, chorioamnionitis, soft tissue infection, and septic thrombophlebitis | All major pathogens can cause such direct extraintestinal infections, including Salmonella, Shigella, Yersinia, Campylobacter, Clostridium difficile |